Epistaxis is a complaint that is frequently seen in the emergency department. As a physician, we took an oath to do no harm, but what if we end up doing more harm than good when managing epistaxis?
A rarely seen reflex that humans possess is the Trigeminocardiac Reflex (TCR). For the emergency physician, the reflex is likely encountered after nasal passage manipulation, such as insertion of a rhino rocket, nasal swabbing, and NG tube placement. If activated, the reflex can lead to rapid hemodynamic instability and death. We want to bring awareness to the reflex and expose the dangers that can come with it. Most clinicians will never come across it in their careers, and if they do, they may fail to even recognize it. In this case report we present a 91-year-old male who presented to our ED with epistaxis who quickly decompensated after rhino rocket insertion.
Case
A 91-year-old gentleman with a history of CAD, hypertension, and NIDDM on aspirin and clopidogrel presented to the ED for a repeat visit with sudden onset of epistaxis from his left nostril that started 2 hours prior to arrival with no evidence of trauma or nasal manipulation. Patient had just arrived back home from a visit from the ENT office, where he had cauterization performed for a right nostril epistaxis with successful hemostasis. He then developed left nostril epistaxis, which led him back to the ED. Upon arrival, the patient had continuous bleeding from the left nostril with unsuccessful hemostasis using nasal clamping. His initial vital signs were stable and as follows: BP 152/66, Pulse of 89, Temp of 36.8 C, and SpO2 of 95%.
The patient continued to have copious amounts of bleeding passing by the nasal clamp and had expectorated out several clots of blood from the oropharynx. The decision was made to apply a 7.5 cm Rhino rocket nasal pack in the left nostril, saturated with tranexamic acid (TXA) followed by the administration of nebulized TXA in a 1:1 solution with normal saline. Approximately 35 minutes after administration of the nasal packing, the patient started to clinically deteriorate. He appeared to be in severe distress, with physical examination findings significant for diaphoresis, cool, and clammy skin. The patient was disoriented and minimally responsive to verbal stimuli. Vital signs revealed a blood pressure of 75/48 mmHg, sinus bradycardia at 55 bpm, and bradypnea. An instinctive response from the resident physician prompted him to immediately remove the nasal packing, and an IV was established for the patient with administration of 1 L Normal Saline and an H/H and type and screen were obtained. The patient was also placed on continuous cardiac monitoring.
Patient clinically improved within 5 min after the removal of the nasal packing. He was no longer disoriented, clammy, or diaphoretic. He had significant improvement of his blood pressure at 115/60 mmHg and resolution of his bradycardia and bradypnea. He did not recall the events that had transpired. Patient’s hemoglobin came back within normal limits and the patient was monitored for 3 more hours in the ED and remained asymptomatic during the rest of his stay and was subsequently discharged to follow up with ENT.
Discussion
So, what happened to our patient? Activation of the trigeminocardiac reflex brings about an overstimulation of the parasympathetic nervous system leading to several potentially life-threatening hemodynamic changes such as bradycardia, hypotension, apnea, and even asystole1. Florian Kratschmer (1843-1922) was the first researcher to provide a comprehensive analysis of changes in breathing, blood pressure, and heart rate that can occur when mucosa of the nasal airways are stimulated mechanically or chemically. Based on the studies completed by Kratschmer, the reflex was ultimately named the Kratschmer reflex or trigeminocardiac reflex (TCR)3. Figure 1 is a drawn-out sketch to represent the reflex.
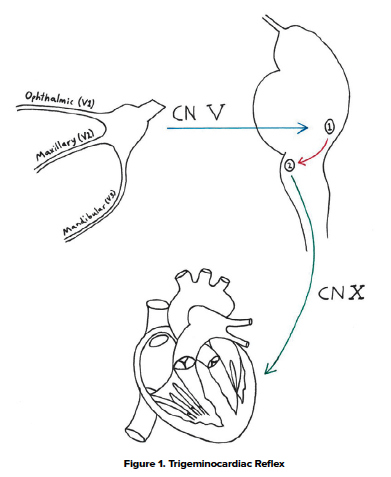
You will notice that nasal packing can stimulate the maxillary branch of the Trigeminal Nerve (Labeled V2), and via CN 5 (blue arrow) results in activation of the main sensory nerve nucleus of Cranial Nerve 5 (Labeled 1). This ultimately sends signals down the internuncial fibers (red arrow) to the motor nucleus of Cranial Nerve 10 (Labeled 2) resulting in an activation of vagal myocardial depressor fibers via CN 10 (green arrow) which leads to an overwhelming hyper-parasympathetic response.4 The reflex is usually witnessed during skull-base surgeries, facial, and dental surgeries, but in the emergency department, this reflex can be elicited via utilization of nasal packing for epistaxis.
Literature documenting outcomes are limited at this time. However, there was a case that was noted. In a 2015 case report by Awasthi et. al, they discussed a patient who became agitated within 15-20 minutes after a posterior nasal packing. The patient then developed hypotension, bradycardia, then subsequently apnea and asystole. Advanced cardiac life support was initiated but the patient failed to achieve return of spontaneous circulation and died. The nasal packing remained in place and was never removed during the cardiac arrest.4
A scarcity in current literature regarding this phenomenon is due to the inability to accurately document the neuroanatomy of this reflex coupled with the rare and variable expression of this in humans beyond the current anecdotal findings by craniofacial surgeries. Significant literature is also unavailable regarding the stimulation of the reflex after nasal packing, but it is a reflex we should know exists and know how to respond when it occurs.
Conclusion
The quintessential significance about the TCR is that immediate removal of the nasal packing or other nasal foreign body will reverse the hemodynamic instability. Fluid boluses will help with hypotension but will not be effective without removing the offending agent. Other differentials for such a clinical presentation could be hemorrhagic shock from massive blood loss or septic shock from toxic shock syndrome. However, these changes would take time to progress and would not cause the immediate hemodynamic instability seen with the reflex. Our objective in presenting this case study is to spread awareness of the unlikely but deadly consequence that nasal packing can cause to your patients, and most importantly, knowing how to reverse it.
References
- Fairbanks DN. Complications of nasal packing. Otolaryngol Head Neck Surg. 1986;94(3):412-415.
- Kratschmer F. On reflexes from the nasal mucous membrane on respiration and circulation. Respir Physiol. 2001;127(2-3):93-104.
- Abdulazim, Amr & Stienen, Martin & Sadr-Eshkevari, Pooyan & Prochnow, Nora & Sandu, Nora & Bohluli, Behnam & Schaller, Bernhard. (2012). Trigeminocardiac Reflex in Neurosurgery – Current Knowledge and Prospects. Explicative Cases of Controversial Issues in Neurosurgery New York: InTech. 10.5772/29607.
- Awasthi D, Roy TM, Byrd RP Jr. Epistaxis and Death by the Trigeminocardiac Reflex: A Cautionary Report. Fed Pract. 2015;32(6):45‐



