Disclaimer
The views expressed herein are those of the authors and do not necessarily reflect the views of the Department of Defense, the Defense Health Agency, the United States Army, or Carl R. Darnall Army Medical Center.
History of Present Illness
A 23-year-old female, G3P2002, at an estimated 6 weeks gestation by last menstrual period, presented to the emergency department for vaginal bleeding and abnormal cramping. Of note, this patient had a known history of uterine didelphys and gave birth 4 months prior to visit. Her method of postpartum birth control was the Depo-Provera shot 4 months prior to visit. The patient denied any other significant past medical history.
Pertinent Physical Exam Findings
The patient had lower abdominal pain to palpation and brisk continuous bleeding from an open cervical os on pelvic exam. Of note, although the patient had two cervixes, pelvic exam was notable for one elongated cervical os.
Pertinent Laboratory Findings
Complete blood count was significant for a lack of anemia, leukocytosis, or thrombocytopenia. Comprehensive metabolic panel was similarly unremarkable. Quantitative beta HCG, however, was significantly elevated at 154,652.9 mIU/mL.
Clinical Question 1
Does this patient have normal quantitative beta HCG for her reported gestational age?
Answer:
No, this patient's quantitative beta HCG is three times the upper limit of normal for 6 weeks gestation.
Clinical Question 2
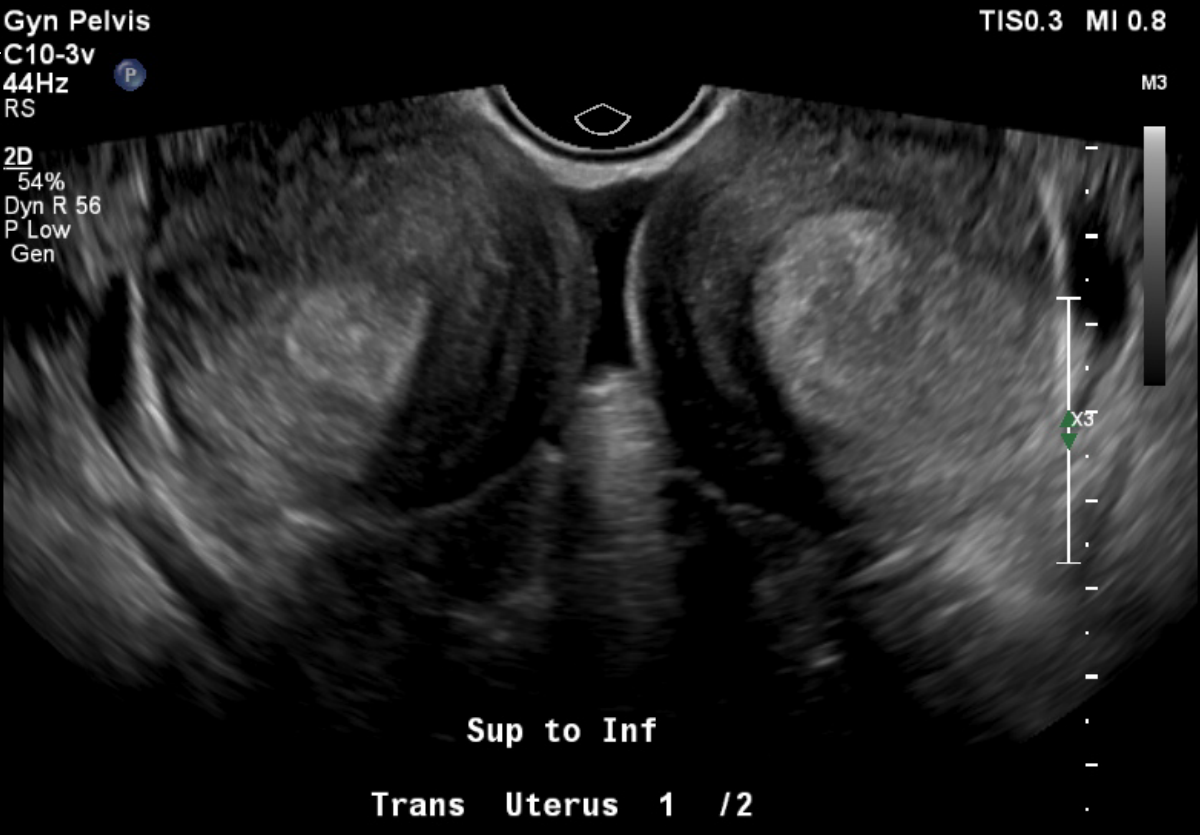
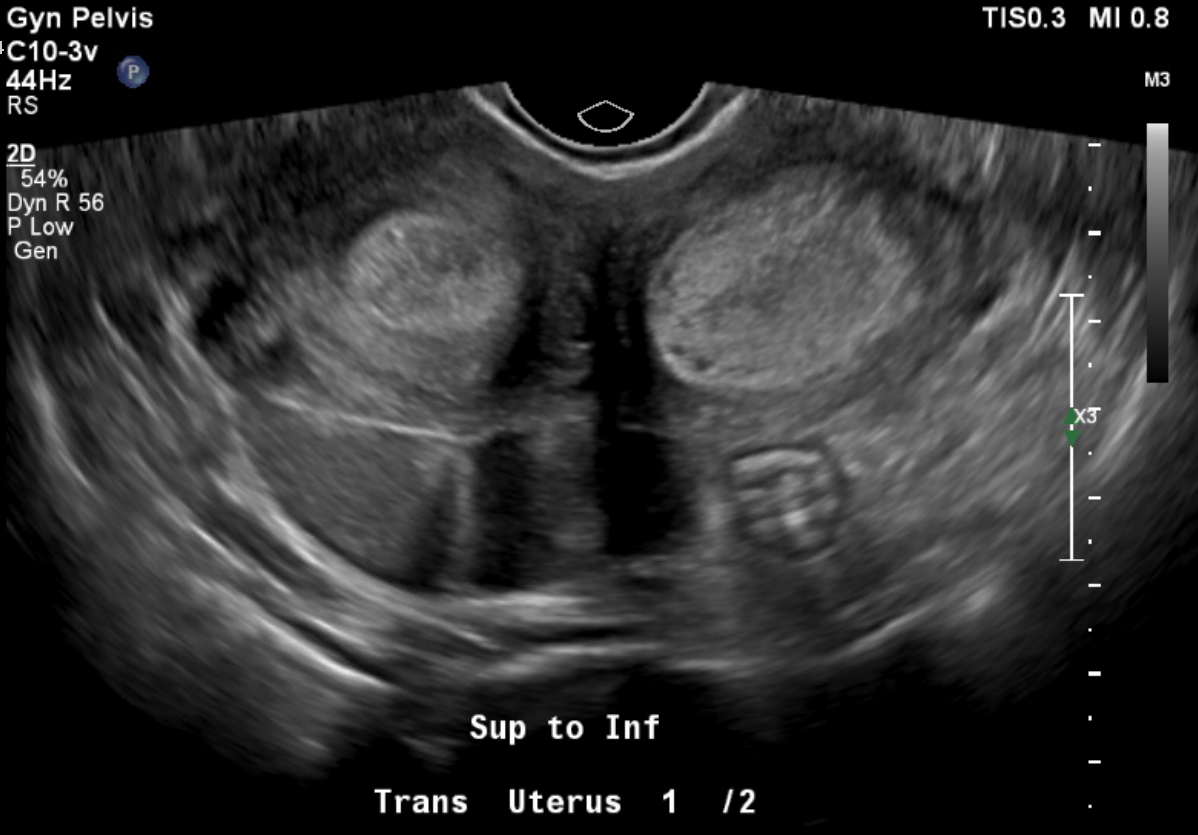
Does this patient have a normally developing pregnancy by ultrasound?
Answer:
No, the snowstorm appearance in both uterine cavities is not consistent with her quantitative hcg; there is also no evidence of a gestational sac or normal intrauterine pregnancy.
Clinical Question 3
What further diagnostic imaging might you obtain?
Answer:
Chest x-ray; if this patient has choriocarcinoma, the most likely metastatic site is the lungs, as it metastasizes hematogenously.
Case Conclusion
Obstetrics/Gynecology were consulted for management given high clinical susion for gestational trophoblastic disease, and recommended chest x-ray and admission for likely dilation and curettage. Chest x-ray was unremarkable, and the patient had successful dilation and curettage of both uterine cavities.
Further pathology of this patient’s uterine contents revealed immature chorionic villi in the left uterine horn with endometrial tissue in the right uterine horn. The report also specified that a very early complete hydatidiform mole and invasive mole must be ruled out, therefore lacking a definitive diagnosis. Clinically, the presentation was consistent with a molar pregnancy.
Case Discussion
This patient had two uncommon pathologies: presumed gestational trophoblastic disease and uterine didelphys. Gestational trophoblastic disease encompasses a spectrum of premalignant to malignant gestational tissue. Rates are difficult to obtain, as there seems to be wide temporal variation, but estimates for hydatidiform mole in particular are estimated to be between 0.57 and 2 per 1000 pregnancies. Ultrasound and laboratory findings such as quantitative beta HCG are mainstays of early identification and treatment. Ultrasound is not very sensitive as a diagnostic modality, but it does have high positive predictive value.1 In this patient, the mismatch in quantitative beta HCG value, last menstrual period date, ultrasound findings, as well as the patient’s postpartum period combined with depo-provera birth control led our team to be exceedingly concerned for gestational trophoblastic disease (GTD). Unchecked, GTD can lead to increased uterine size and bleeding, to endocrine abnormalities, and even to invasive central nervous system lesions and death; however, with treatment and early diagnosis complete resolution nears 100% in women.2 It is important to remember to include a chest x-ray in your workup for screening in a patient with suspected gestational trophoblastic disease to determine staging and appropriate treatment. For example, if lung lesions are visible, the patient would require CT Chest/Abdomen/Pelvis and brain MRI to determine staging.3 If found to have metastatic disease, these patients likely need chemotherapy.4 This changes the level of subspecialty care the patient needs.
In addition to gestational trophoblastic disease, this patient had a congenital uterine anomaly. Uterine didelphys is one phenotype of a spectrum of congenital uterine anomalies. These originate from failure of the mullerian ducts to completely fuse and range from this patient’s two separate uteruses and cervixes, to a bicornuate uterus morphology, to a uterine septum. Congenital uterine anomalies have a rate of 4.3–6.7%. The spontaneous abortion rate is increased in people with congenital uterine anomalies. One explanation is that, for a septate uterus in particular, a blastocyst can implant on the septum, which may not be robust enough to support further growth and development.5 Although this particular patient knew about her preexisting condition prior to emergency department presentation, it is within reason that we may be the first to diagnose this condition in a patient dealing with their first pregnancy, and subsequently, we are obligated to disclose this anomaly when we find it, and hopefully provide some information to the patient regarding potential risks.
As an Emergency Medicine provider, what implications does this photo and case have?
Key Take-Aways
- When you see an abnormally high quantitative beta hCG finding for gestational age, an ultrasound and follow up are necessary to prevent further morbidity and mortality.
- When you see an abnormal uterus, know associated pregnancy complications so that you can counsel your patient and encourage early prenatal care.
- When bleeding during early pregnancy occurs, an open cervical os indicates inevitable abortion/miscarriage.
- A patient with uterine didelphys can have two separate IUPs with different gestational ages.
References
- Chawla T, Bouchard-Fortier G, Turashvili G, et al. Gestational trophoblastic disease: An update. Abdom Radiol 48, 1793–1815 (2023).
- Bishop BN, Edemekong PF. Choriocarcinoma. [Updated 2023 Feb 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
- Gestational Trophoblastic Neoplasia. National Comprehensive Cancer Network. Updated 2025-05-28.
- Horowitz NS, Eskander RN, Adelman MR, Burke W. Epidemiology, Diagnosis, and Treatment of Gestational Trophoblastic Disease: A Society of Gynecologic Oncology Evidenced-Based Review and Recommendation. Gynecologic Oncology. 2021;163(3):605-613.
- Venetis CA, et al. "Clinical implications of congenital uterine anomalies: a meta-analysis of comparative studies." Reprod Biomed Online, 29.6. 2014; 665-683.



