Lung injuries associated with electronic cigarettes (aka vaping) are on the rise, especially among teens. With a higher risk of addiction and weaker regulations, vaping can be cause for concern.
Case
A 17-year-old male with a history of chronic abdominal pain presented to the emergency department with 2 weeks of worsening abdominal pain and diarrhea. His CT scan showed possible early appendicitis and incidental findings of bibasilar ground glass opacities in the lungs. Stool studies were positive for Clostridium difficile (C.diff) and enteropathogenic Escherichia coli (EPEC), and laboratory work-up revealed elevated inflammatory markers and leukocytosis. He had no respiratory complaints and had normal saturations on room air. He was diagnosed with colitis and discharged home on oral metronidazole. Two days later, the patient returned to the ED with worsening abdominal pain and fever. He had oxygen saturations of 91% on room air and a respiratory rate of 28. A chest x-ray showed diffuse interstitial lung markings (Figure 1), and a chest CT showed extensive ground glass alveolar opacities (Figure 2). The patient was started on supplemental oxygen and admitted.
Figure 1. Diffuse interstitial lung markings in both lungs on chest x-ray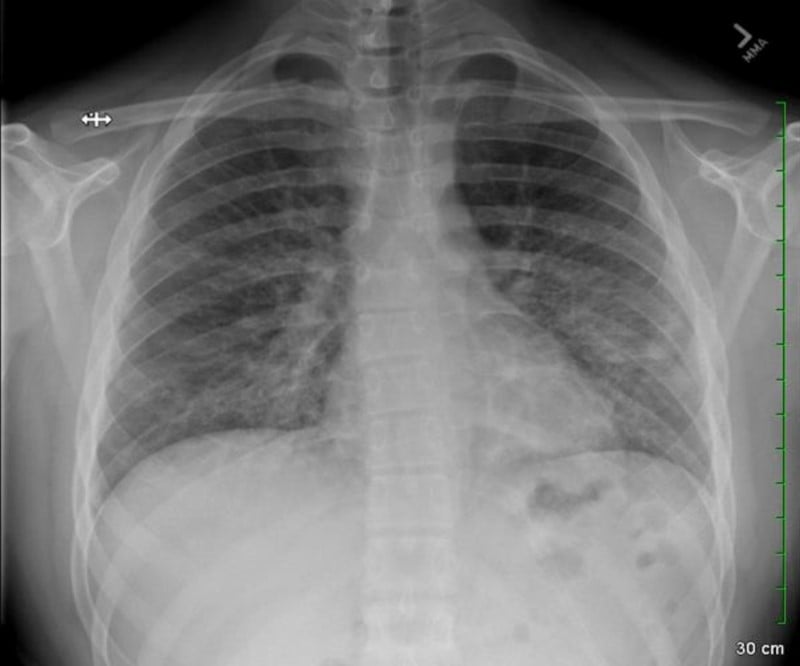
Figure 2. Extensive interstitial and more notably alveolar ground glass opacities in a patchy distribution in both lungs on chest CT
Vaping: An Epidemic in Teenagers
In the time before COVID-19, electronic cigarette use, or vaping, occupied the airwaves as an emerging public health concern, particularly within pediatric and adolescent populations. Considered to be an alternative to traditional cigarettes and marijuana smoking, vaping is a smoking method that involves heating a liquid so that it aerosolizes and can be subsequently inhaled. The liquid itself contains various different toxins, including highly concentrated amounts of nicotine, cannabis-derived extract, propylene glycol, vegetable glycerin, acrolein, formaldehyde, ethanol, and menthol which provides flavoring.2-4
Vaping can be performed through a variety of devices, all of which are made differently depending on the users' needs. For example, there are newer generations of products that are longer lasting, are reusable, and have the potential to deliver higher amounts of nicotine than earlier generation devices.
In the more recent years, there has been an up-trend of vaping product purchases within the adolescent population, as vaping use rose up to nearly 8% (approximately 1.3 million teenagers) between 2017-2019. Not only do weaker FDA regulations on e-cigarette and vaping devices contribute to these findings,5 social media, too, is another influential factor.6-10 One study found that > 78% of middle and high-school aged students were exposed to at least one vaping advertisement.11 Other studies revealed that flavor is one of the most appealing qualities of vapine, and therefore producers have created an assortment of eye-catching vaping devices that offer fruit and candy flavors.12-13
Addiction with vaping occurs much faster than combustible cigarettes; while addiction occurs with the daily consumption of four to five traditional cigarettes, this is equivalent to only a quarter of the amount within a JUUL pod.14 Contributing to the dependency on these products is the higher concentration of nicotine found in vaping devices compared to traditional nicotine products. A recent study by University of California, San Francisco found that blood nicotine concentrations in the JUUL group was 5.2 times higher than traditional cigarettes.15
Therefore, it is critical to recognize the risk factors, histories, and presentations of patients to treat E-cigarette or Vaping Associated Lung Injury (EVALI) to avoid long term health complications.
E-Cigarette or Vaping Use-Associated Lung Injury (EVALI): A Diagnosis of Exclusion
Despite EVALI becoming more prevalent in our society, our understanding behind its underlying pathophysiology remains unclear. There are no specific symptoms, imaging modalities, or markers that directly lead to its diagnosis.16 Although it is more common for EVALI to present with respiratory symptoms, there have been case series showing that it can, too, manifest as gastrointestinal and constitutional complaints. In one case study, patients identified with EVALI were often white males with a median age of 21 who presented with shortness of breath (85%) and cough (85%). Subjective fever (84%) and chills (60%) were also common in these patients, as well as nausea (66%), vomiting (61%), diarrhea (44%), and abdominal pain (34%). Patients were also generally found to be tachycardic and, on lab studies, had increased inflammatory markers and a leukocytosis. It should be noted that 100% of patients in this study were found to have bilateral infiltrates on chest CT, which, along with the patients’ histories, aided the ED staff in deriving the diagnosis.17
Given EVALI's non-specific presentations, it is critical to maintain a high index of suspicion to ensure these cases are diagnosed early. This involves the emergency healthcare provider screening adolescents with non-specific symptoms for EVALI. By assessing vaping history and risk factors including social and environmental factors, smoking history, drug use history, and family stressors, such as having divorced parents,11 during initial patient encounters, EM physicians with heightened suspicion can expand their differential and start treatment before respiratory decompensation occurs.
Identifying presentations and creating guidelines for the evaluation and care of pediatric and adolescent patients is necessary to reduce the morbidity and mortality that has been associated with vaping. As of December 2019, there have been over 2,000 hospitalized EVALI cases and 48 deaths reported, highlighting the significance of its rise to prominence as EVALI was only first described in 2019.15 With the recent rise in the number of cases, much has been done to develop these guidelines; however, these do not fully encompass the wide variety of ED presentations with EVALI.18 In order to screen these patients, it may be advisable to complete chest imaging (either x-ray or CT) in patients with non-specific presentations and significant vaping use. The exact pathogenesis and progression of this new disease are still being researched and may allow for more specific screening protocols as more information is uncovered.
Current treatment guidelines center on attempting to treat the overlying pneumonia with antibiotics based on community-acquired pneumonia guidelines, bacterial isolates, and clinical suspicion. Additionally, starting systemic steroids has shown promise in inpatient treatment, but has yet to be adequately studied in the outpatient setting.19 In general, it is advisable to discharge patients with EVALI to complete outpatient workup and management if:
- O2 saturation >95%
- There is no respiratory distress
- There are no comorbidities that compromise pulmonary reserve
- The patient has reliable access to care with a 24-48 hr follow-up
- The patient has strict return precautions
In addition, organizing plans to quit and giving resources to help patients overcome their dependence is extremely important to prevent additional progression of the disease. As this is a new and developing disease, reporting cases to local health departments for further study is also encouraged by the CDC.
Back to Our Patient
While recent reports show that 77% of patients with EVALI have gastrointestinal symptoms, as was experienced by our patient, it is rare for these to be present without concomitant respiratory symptoms.17
Our patient's GI symptoms and respiratory distress worsened early on in his course, leading to a temporary stay in the pediatric intensive care unit (PICU) where he needed additional respiratory support in the form of bilevel positive airway pressure (BIPAP). His antibiotics were broadened for empiric treatment of other potential intra-abdominal pathology.
After obtaining a more extensive history, the patient admitted to a 2-year history of vaping. His product of choice was JUUL e-cigarettes, and he smoked approximately one nicotine pod daily. He admitted to smoking marijuana as well, but denied smoking synthetic marijuana or using marijuana containing pods in e-cigarettes. After these revelations, the patient was subsequently started on high dose intravenous methylprednisolone. Over the next 48 hours, the patient improved clinically, and he was weaned off BIPAP to room air within 72 hours. He was discharged home on prednisolone and fluticasone propionate therapy and was counselled extensively on the effects of vaping and lung related injuries, as well as the need for continued pulmonology follow up.
Conclusion
While vaping has disappeared from the forefront of our collective minds in light of recent global pandemics, its place in and effect on pediatric populations is not going anywhere anytime soon. Vaping-induced lung injury is a new diagnosis that has increased drastically in prevalence as the popularity of electronic cigarettes, or vaping, has grown at an incredible rate. Many users are not aware of the harms this practice can do to the body, and furthering knowledge about the consequences may be able to prevent disease.
EM physicians should have a high index of suspicion for electronic cigarette use in adolescents presenting with gastrointestinal symptoms with no pertinent history, and it is imperative that we continue to examine the syndrome as its prevalence rises.
References
- Richter L. What parents should know about the different vaping devices. Center on Addiction. https://www.centeronaddiction.org/e-cigarettes/recreational-vaping/what-parents-should-know-about-different-vaping-devices. Published 2018. Accessed May 30, 2020.
- DeVito EE, Krishnan-Sarin S. E-cigarettes: Impact of E-liquid Components and Device Characteristics on Nicotine Exposure. Current Neuropharmacology. 2018;16(4): 438-459.
- Davidson K, Brancato A, Heetderks P, et al. Outbreak of Electronic-Cigarette-Associated Acute Lipoid Pneumonia - North Carolina, July-August 2019. MMWR Morb Mortal Wkly Rep. 2019;68(36):784‐786. Published 2019 Sep 13.
- Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2016; 9: Cd010216.
- U.S. Food and Drug Administration. The Facts on the FDA's New Tobacco Rule. Published June 2016. Accessed May 30, 2020.
- Miech R, Johnston L, O'Malley P, et al. Trends in Adolescent Vaping 2017-2019. N Engl J Med. 2019; 381:1490-1491.
- Jones K, Salzman GA. The Vaping Epidemic in Adolescents. Mo Med. 2020;117(1):56‐58.
- Farzal Z et al. The Adolescent Vaping Epidemic in the United States - How It Happened and Where We Go From Here. JAMA Otolaryngol Head Neck Surg. 2019;145(10):885-886.
- Cherian SV, Kumar A, Estrada-Y-Martin RM. E--cigarette or Vaping- Product Associated Lung Injury: A Review. Am J Med. 2020 Mar 13. pii: S0002-9343(20)30140-6.
- Watkins NK, Ohannessian CM. Timing of Vape Use Among Adolescents: Differences by Family Structure. Drug Alcohol Depend. 2020 Apr 1;209:107953.
- Slekman J. Vaping: It’s all a smokescreen. Pediatric Nursing. 2019;45(1):12-15,35. .
- Tobore TO. On the Potential Harmful Effects of E-Cigarettes (EC) on the Developing Brain: The Relationship Between Vaping-Induced Oxidative Stress and Adolescent/Young Adults Social Maladjustment. J Adolescence. 2019;76:202-209.
- Leventhal AM, Goldenson NI, Cho J, et al. Flavored E-cigarette Use and Progression of Vaping in Adolescents. Pediatrics. 2019;144(5).
- Jackler, R.K. & Ramamurthi, D. Nicotine arms race: JUUL and the high-nicotine product market. Tobacco Control. 2019;28:623-628.
- Rao P, Liu J, Springer ML. JUUL and Combusted Cigarettes Comparably Impair Endothelial Function. Tobacco Regulatory Science. 2020;6(1):30-37.
- Triantafyllou GA, Tibero PJ, Zou RH, Lamberty PE, et al. Vaping-Associated Acute Lung Injury: A Case Series. Am J Respir Crit Care Med. 2019 Dec 1;200(11):1430-1431.
- Layden JE, Ghinai I, Pray I, et al. Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin - Final Report. N Engl J Med. 2020 Mar 5;382(10):903-916.
- Evans ME, Twentyman E, Click ES, et al. Update: Interim Guidance for Health Care Professionals Evaluating and Caring for Patients with Suspected E-cigarette, or Vaping, Product Use-Associated Lung Injury and for Reducing the Risk for Rehospitalization and Death Following Hospital Discharge - United States, December 2019. MMWR Morb Mortal Wkly Rep. 2020;68(5152):1189‐1194. Published 2020 Jan 3.
- Siegel DA, Jatlaoui TC, Koumans EH, et al. Update: Interim Guidance for Health Care Providers Evaluating and Caring for Patients with Suspected E-cigarette, or Vaping, Product Use Associated Lung Injury — United States, October 2019. Morbidity and Mortality Weekly Report. 2019;68:919–927.



