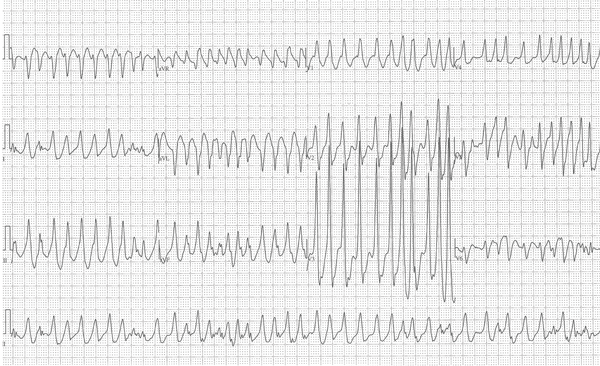
A healthy 28-year-old male with no past medical history presents to the emergency department with palpitations and dizziness. Vital signs are within normal limits except for a recorded heart rate of 220 bpm. An ECG is obtained (Figure 1).
Questions to Consider
- What is the rhythm?
- What treatment options must you consider?
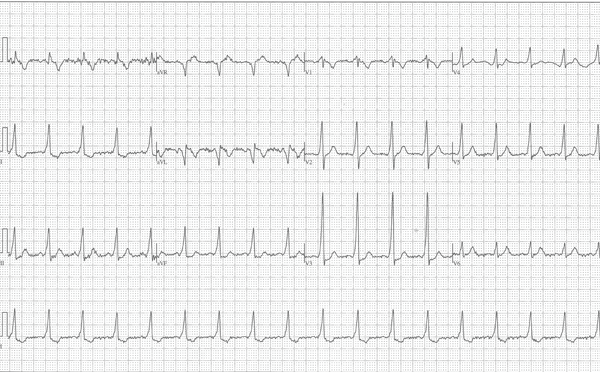
There is a concern for atrial fibrillation (AF) with pre-excitation from an accessory pathway. Defibrillation pads are placed on the patient, and the decision is made to electrically cardiovert. A post-cardioversion ECG confirms the suspected diagnosis of AF with Wolff-Parkinson-White (WPW) (Figure 2).
Discussion
The first step in managing this potentially critical patient is to correctly identify the presenting rhythm. Ask yourself three simple questions:
- Is the rate fast or slow?
- Is the rhythm regular or irregular?
- Is the QRS complex wide or narrow?
By asking yourself these simple questions off the bat, you will diagnose this rhythm as an irregular wide complex tachycardia. The differential diagnosis for an irregular wide complex tachycardia (WCT) includes polymorphic ventricular tachycardia (PVT); AF with aberrant conduction (bundle branch block or non-specific intraventricular conduction delay); and AF with pre-excitation (WPW).1
How do we know this is AF with WPW? In normal physiological cardiac conduction, an impulse is generated at the sinus node and travels to the AV node, resulting in atrial contraction (P wave). A conduction delay at the AV node (PR interval) allows the ventricles to fill. Finally, the ventricles are depolarized via the His-Purkinje system (QRS complex), and the ventricles simultaneously contract. In WPW, initial depolarization of the ventricle results via an accessory pathway known as the bundle of Kent. The early activation of the ventricle results in a shortened PR interval and a slow initial upstroke of the QRS complex. This occurs while the rest of the signal propagates normally through the AV node. Thus, a shortened PR interval, a widened QRS, and a delta wave make up the classic triad seen in WPW.2
In AF with WPW, some of the atrial impulses travel down the normal pathway, while others travel down the accessory pathway. This results in a recognizable ECG that is distinct from other irregular WCTs in several important ways. First, because of the accessory pathway, the rate is >200 bpm and at times approaches 300 bpm. Second, because of simultaneous conduction through both the accessory pathway and the His-Purkinje system, the QRS complex is wide (>0.12 seconds) and has varying bizarre morphologies. Finally, the axis is stable and not undulating, which differentiates it from PVT.1
Treatment
It is imperative to recognize AF with WPW, as incorrect treatment with AV nodal blocking agents can be fatal. Blocking the AV node in these patients will result in preferential use of the accessory pathway. Rates may exceed 300 or 400 bpm and are at extreme risk for degeneration into ventricular fibrillation (VF). Thus, an irregular wide complex tachycardia with rates approaching 300 bpm, bizarre and varying QRS morphologies, and a stable axis, must be treated as AF with WPW until proven otherwise. Procainamide (50-100 mg every 2 min to a max dose of 17 mg/kg) or ibutilide (0.01 mg/kg maximum 1 mg over 10 min) are the treatments of choice for chemical conversion.4 Amiodarone is controversial but has been known to cause decompensation into VF, due to its calcium-channel blocking and beta-blocking effects.5 Electrical cardioversion is the treatment of choice for unstable patients, however it is also an acceptable treatment for stable patients. Finally, it is recommended that cardiology be involved early to further guide your treatment decisions.
Other Tachyarrhythmias
Because of the accessory pathway, WPW can also present as an atrioventricular reentrant tachycardia (AVRT). Orthodromic AVRT is a regular narrow complex tachycardia, whereas antidromic AVRT is a regular wide complex tachycardia. Note that regularity distinguishes both of these rhythms from AF.
In orthodromic AVRT, an impulse leaves the SA node, travels normally through the AV node, and then back to the atria through the accessory pathway. In antidromic AVRT, the impulse travels from the SA node to the accessory path first, and then travels back to the atria via the AV node. Ventricular depolarization via the accessory pathway occurs slowly and results in a widened QRS complex.3
WPW with orthodromic AVRT looks identical to run-of-the-mill paroxysmal supraventricular tachycardia (SVT) and can be treated as such. Vagal maneuvers or AV nodal blocking agents are the treatment of choice, as they slow conduction through the AV node and disrupt the re-entrant circuit. On the other hand, WPW with antidromic AVRT will look identical to ventricular tachycardia (VT). Since it is virtually indistinguishable, it should be treated with procainamide, amiodarone, or electrical cardioversion in the case of an unstable patient.1
References
- Brady WJ, Truwit JD. Critical Decisions in Emergency & Acute Care Electrocardiography. Hoboken, NJ: Wiley Blackwell; 2009:252-255; 295-302.
- Burns E. Life in the Fast Lane. Pre-excitation Syndromes. http://lifeinthefastlane.com/ecg-library/pre-excitation-syndromes. 2012.
- Piktel J. Cardiac Rhythm Disturbances. Tintinalli's Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill. 2011:129.
- Fengler BT, Brady WJ, Plautz CU. Atrial fibrillation in the Wolff-Parkinson-White syndrome: ECG recognition and treatment in the ED. Am J Emerg Med. 2007;25(5):576-83.
- Simonian SM, Lotfipour S, Wall C, Langdorf MI. Challenging the superiority of amiodarone for rate control in Wolff-Parkinson-White and atrial fibrillation. Intern Emerg Med. 2010;5(5):421-6.