CASE
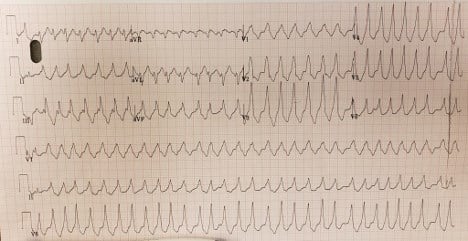
A woman in her 40s presented to the emergency department with a chief complaint of palpitations. What is your interpretation of her ECG?
ANSWER
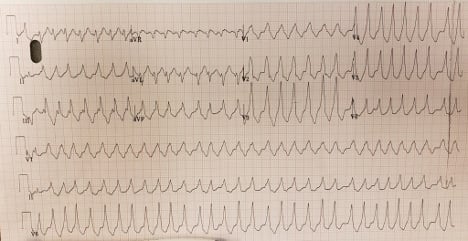
The rate is clearly fast; it varies between just over 1 big box wide to about 2 big boxes wide, so it’s somewhat irregular. By counting the complexes in the strip, there are 32 QRS complexes, which, multiplied by 6, determines a rate of approximately 180 bpm. We see that it is also wide complex. The differential for irregular wide complex tachycardias is not broad. Ventricular tachycardia (VT) is a possibility, but monomorphic VT is usually relatively regular (and would be unusual in a relatively young person). Polymorphic Vtach is usually a pre-terminal rhythm in patients with significant heart disease. Atrial fibrillation (AFib) with LBBB is on the differential. However, the LBBB QRS morphology is pretty stereotyped; you typically don’t see different wide QRS complexes, you just see the same wide QRS. In this case, in lead III as well as aVL, there are some complexes that are different from their neighbors. The rate also tips us away from AFib with LBBB, which is limited by the AV node; rates in the 180s would be atypically fast for AFib complicated only by LBBB. All of this should lead us to think about the third possibility, AFib with Wolff-Parkinson-White syndrome (WPW.)
The axis looks to be right, the QRS is wide, and the ST segments are generally depressed, which is to be expected with a rate this fast and wide.
So how would we treat this patient? Her blood pressure was tolerating the rhythm reasonably. When it was determined that AFib with WPW was a real possibility, the team opted to treat with procainamide. This is the ECG 30 minutes post-treatment:
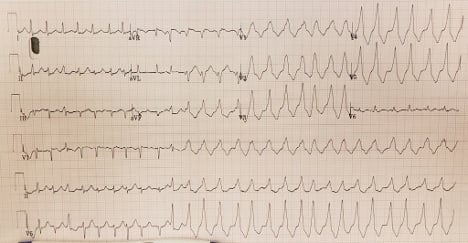
We see the patient remained in AFib, but now was alternating between ortho- and antidromic conduction; the first half of the EKG was narrow complex. Interestingly, looking at the narrow complex section, we see a slightly wider complex beat demonstrating the classic delta wave pattern of WPW:
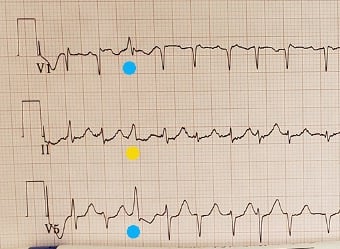
It’s not uncommon for WPW patients to only intermittently show the delta wave, which means an old normal ECG does not rule out the diagnosis.4
It is important to note that, while AFib with WPW may not be the most common cause for irregular, wide-complex tachycardia, AFib does occur in 20% of patients with WPW due to the presence of an accessory pathway that allows for rapid conduction directly to the ventricles bypassing the AV node. This needs to be recognized when it occurs, because the AV nodal blocking agents that we would typically give for AFib (such as adenosine), preference conduction via the accessory pathway and can lead to degeneration into VT or ventricular fibrillation.1
CASE CONCLUSION
With another 30 minutes on the procainamide drip the patient converted back to sinus rhythm.
LEARNING POINTS
- The differential for an irregular wide-complex tachycardia includes polymorphic VTach, AFib with LBBB (aka AFib with aberrancy), and AFib with WPW.
- Patients with WPW have an accessory pathway that disrupts isolation between atria and ventricles and allows electrical impulses to bypass the AV node.2
- The hallmark of WPW is a short PR interval and prolonged QRS with an initial slurring upstroke, or “delta” wave, although this is not universally present on all ECGs of patients with WPW.2
- Administering AV nodal blocking agents to patients in AFib with WPW can lead to ventricular arrhythmias and cardiac arrest.
- Treatment for AFib in WPW is procainamide of ibutilide if stable, and electrical cardioversion if unstable.3