A 57-year-old man presented to the emergency department with palpitations and a sensation of nervousness after alcohol consumption. He had no history of angina or myocardial infarction.
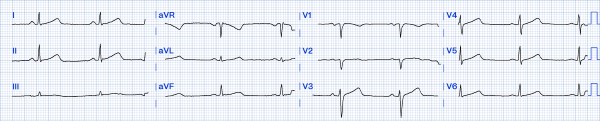
On examination, his blood pressure was unmeasurable due to hemodynamic instability. Oxygen saturation was 98% on pulse oximetry, and cardiac monitoring showed a regular tachycardia at 240 beats per minute. (Figure 1)
Figure 1. Initial ECG
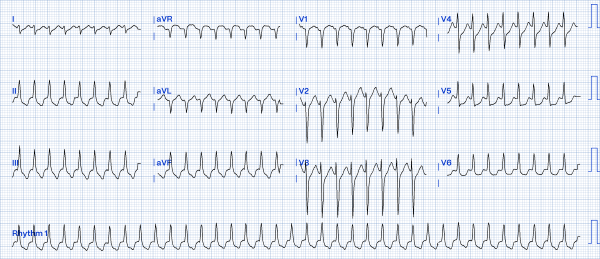
After the patient underwent synchronized cardioversion, sinus rhythm was immediately restored. (Figure 2)
Figure 2. ECG after cardioversion
 Further evaluation was performed, revealing hypokalemia with a serum potassium level of 2.9 mmol/L. Other laboratory tests, including troponin, inflammatory markers, and thyroid function were unremarkable.
Further evaluation was performed, revealing hypokalemia with a serum potassium level of 2.9 mmol/L. Other laboratory tests, including troponin, inflammatory markers, and thyroid function were unremarkable.
DISCUSSION
The first ECG showed a regular narrow-complex tachycardia with no obvious P waves and regular R-R intervals.
The differential diagnoses include:
- Atrioventricular nodal reentrant tachycardia (AVNRT)
- Atrioventricular reentrant tachycardia (AVRT)
- Ectopic atrial tachycardia
- Atrial flutter 2:1 conduction
- Sinus tachycardia
Sinus tachycardia:
Defined by steady rhythm with P waves before each QRS complex. This is unlikely in our case. The ECG rate of 240 bpm is faster than the sinoatrial node can deliver an impulse. Moreover, there are no visible P waves preceding each QRS complex.1
Atrial tachycardia:
A form of SVT defined by abnormal p-wave morphology and axis, uniform p-waves, an isoelectric baseline, and normal QRS morphology.
Second, the ECG shows no distinguishable P waves, which makes atrial tachycardia less likely.
Atrial flutter:
Defined by narrow complex tachycardia with loss of the isoelectric baseline and a "saw-tooth" pattern of inverted flutter waves in leads II, III, aVF.
The lack of sawtooth-shaped F waves across the inferior leads and a ventricular rate of 240 beats per minute make atrial flutter 2:1 conduction less likely.
Another important consideration in tachycardia is ventricular tachycardia. However, this presents as a wide complex tachycardia, and atrioventricular (AV) dissociation and capture beats may be present. This is also unlikely given the narrow QRS complexes in our case.
The ECG findings—including a regular rhythm, narrow QRS complexes, a heart rate of 240 bpm, and P waves that may be indistinct or appear after the QRS complex—are consistent with the diagnosis of AVNRT or AVRT.
Since P waves are not visible during the tachycardia episode and the pre-hospital electrocardiogram showed no evidence of Wolff-Parkinson-White (WPW) syndrome, AVRT is unlikely.2 Concurrently, after electrical cardioversion, delta waves characteristic of WPW syndrome remain absent. This ECG study suggests a low-fast variant of AVNRT.3 Wolff-Parkinson-White (WPW) can alter the morphology of the QRS, or it may conceal some accessory pathways, leading to other conduction abnormalities. Therefore, a delta wave may not always be apparent on the resting ECG.
In our case, we suspect alcohol contributed to the patient’s episode of AVNRT. Alcohol is not a direct cause of AVNRT, but it may act as an indirect trigger through several mechanisms, including:4
- Increased catecholamine levels and stimulation of the sympathetic nervous system.
- Electrolyte imbalances (hypokalemia, hypomagnesemia).
In a case-control study, numerically more individuals with SVT were observed in those who consumed >6 drinks per day; however, this was of borderline statistical significance.6
Individuals who consume excess amounts of alcohol can present with excessive vomiting, leading to dehydration and electrolyte imbalance, thereby increasing the risk of triggering cardiac arrhythmias. Thus, intravascular volume replacement is necessary to ensure electrolyte balance to prevent the recurrence of tachyarrhythmia.
CASE CONCLUSION
A patient presented to the emergency department with regular tachycardia, narrow complex, and no distinct P waves observed. After excluding other causes, two main diagnoses were considered: AVNRT and orthodromic AVRT. Prompt electrical cardioversion is critical in hemodynamically unstable patients, as timely intervention is essential to restore sinus rhythm and prevent further complications.
LEARNING POINTS
- Recognizing regular narrow complex tachycardia: QRS complex duration <120 ms.
- Differential diagnosis includes: AVNRT, AVRT, ectopic atrial tachycardia, atrial flutter 2:1 conduction, and sinus tachycardia.
- Atrioventricular nodal reentrant tachycardia (AVNRT): Regular rhythm, heart rate 180-240 bpm, P waves are unclear, possibly buried within the QRS complex or appearing immediately after QRS, the most common cause of regular narrow-complex tachycardia in adults.
- Alcohol as a trigger: Alcohol may act as an indirect trigger through sympathetic nervous system stimulation or electrolyte imbalance (hypokalemia, hypomagnesemia) triggering AVNRT episodes.
- Urgency of treatment: Synchronized electrical cardioversion is the safest and most effective measure in hemodynamically unstable patients.
- Electrolyte correction: Hypokalemia (2.9 mmol/L in this case) should be corrected immediately to prevent recurrence.
REFERENCES
- Surawicz B, Knilans TK. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric. 6th ed. Philadelphia, PA: Saunders/Elsevier; 2008.
- Strauss DG, Schocken DD, Wagner GS. Marriott’s Practical Electrocardiography. Thirteenth edition. Philadelphia: Wolters Kluwer; 2021.
- Hafeez Y, Armstrong TJ. Atrioventricular Nodal Reentry Tachycardia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; August 2023. Accessed March 27, 2025.
- Wong CX, Tu SJ, Marcus GM. Alcohol and Arrhythmias. JACC: Clinical EP. 2023;9(2):266–79. Accessed March 27, 2025.
- Page RL, Joglar JA, Caldwell MA, et al., for the Evidence Review Committee. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia. Circulation. 2015;133(14):e507-e574. Accessed March 27, 2025.
- Wong CX, Tu SJ, Marcus GM. Alcohol and Arrhythmias. JACC: Clinical Electrophysiol. 2023;9(2):266-2793.