Aortic dissection (AD) is part of a group of acute aortic syndromes consisting of intramural aortic hematoma, penetrating aortic ulcer, and aortic rupture.
On its own, the incidence is approximately 3-8 cases per 100,000 per year, and up to 25% of cases are missed. The in-hospital mortality when treated is 27%, with a 2% increase in mortality/hour. Imaging modalities like CT angiography, TEE, and MRA have made improved diagnosis of the disease, but are costly, potentially harmful, time-consuming, and require patient stability when in use.1 The key concern in the ED is if there is a way to risk stratify patients for AD and, if so, is there a test with high enough sensitivity and negative likelihood ratio (-)LR to rule out AD. Smooth muscle myosin heavy chain is a proposed modality, which is released from injured aortic media at the start of AD, but there is a lack of observational studies testing its efficacy as biomarker in diagnosing.2 Hence, an algorithm to help reduce both misdiagnosis and overtesting is much needed.
Literature Review
Plasma D-dimer, a degradation product of cross linked fibrin by the endogenous fibrinolytic system, is found to be elevated in states like cancer, MI, pregnancy, sepsis, or disorders where there is indiscriminant activation of the coagulation cascade.2 Meta-analysis reviews of D-dimer studies have shown that a cut-off level 0.50 ug/mL has proven to have high sensitivity, (-)LR, and negative predictive value.2,3 According to the IRAD-Bio study, when utilized in the first 24 hours of symptoms, D-dimer can reliably rule out pulmonary embolism (PE) and acute AD with sensitivity of 96.6% and specificity of 46.6% studied on AD patients.3,4 Although a rapid, economical, and accessible biomarker, it is also nonspecific with a low specificity and PPV and a poor (+)LR.2 The possibility of excessive advanced imaging is increased when used alone on a low-risk patient population. Therefore, when coupled with a decision rule like the Aortic Dissection Detection Risk Score (ADD-RS), it can provide better utility with increased sensitivity.
Risk Stratification Tool
ADD-RS is a set of 12 clinical markers of aortic dissection released in 2010 by American Heart Association and the American College of Cardiology.5 This scoring system was developed using the International Registry for Aortic Dissection, comparing common historical and clinical features. The strength of the ADD-RS scoring system is that its retrospective analysis of IRAD showed that low risk scores of 0 had a sensitivity for AD of 95.4%. Of the 4.6% that had AD with a score of 0, 48.6% of these patients had abnormal chest radiographs, including things such as widened mediastinum. If considering that these patients would be worked up anyway due to an abnormal chest radiograph, the miss rate of the ADD-RS would be 2.23%.
The ADvISED Trial1 evaluated the ADD-RS combined with D-dimer testing by conducting a multicenter, prospective observational study which enrolled 1,850 consecutive chest pain patients, 241 (13%) of which were diagnosed with acute aortic syndrome (AAS). ADD-RS<=1 and negative D-dimer showed a sensitivity of 98.8%, NPV 99.7%, and LR-0.02. An ADD-RS=0 had a sensitivity of 99.6%. Furthermore, application of this rule could potentially spare ~3 in 5 conclusive imaging exams in all patients with AAS, and could avoid up to 1 in 2 CTA exams in patients with suspected AAS.1
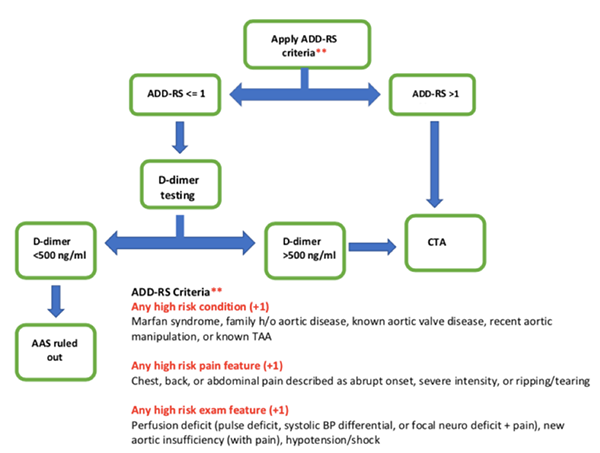
For perspective, a 65-year-old male with known history of TAA presenting with abrupt onset of chest pain radiating to back who appears diaphoretic and hypertensive would immediately receive a CTA based on risk factors and presentation alone. However, a 56-year-old with history of HTN presenting with chest pain radiating to back, but well-appearing and stable vital signs can be appropriately risk stratified with this tool. Her ADD-RS of 0 indicates D-dimer can be obtained. If the level is negative, and she remains hemodynamically stable, we can safely rule out AAS while reducing cost and radiation exposure. This strategy could aid in standardizing decisions on advanced imaging for suspected AAS, while balancing the risks of misdiagnosis and over-testing. This could become an essential tool analogous to Wells Criteria, PERC, and D-dimer. The authors suggest further prospective studies for validation but are optimistic for its future.
Notice This research was supported by HCA and/or an HCA affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA.
References
- Nazerian P, Mueller C, Soeiro AM, et al. Diagnostic Accuracy of the Aortic Dissection Detection Risk Score Plus D-Dimer for Acute Aortic Syndroms: The ADvISED Prospective Multicenter Study. Circulation 2018;137(3):250-258.
- Shimony A, Filion KB, Mottillo S, Dourian T, Eisenberg MJ. Meta-Analysis of Usefulness of D-dimer to Diagnose Acute Aortic Dissection. Am J Cardiol 2011;109(8):1227-1234.
- Asha SE, Miers JW. A Systematic Review and Meta-Analysis of D-dimer as a Rule-out Test for Suspected Acute Aortic Dissection. Ann Emerg Med 2015:66(4):368-378.
- Suzuki S, Distante A, Zizza A, et al. Diagnosis of Acute Aortic Dissection by D-Dimer. Circulation 2009;119(20):2702-2707.
- Rogers AM, Hermann LK, Booher AM, et al. Sensitivity of the Aortic Dissection Detection Risk Score, a Novel Guideline-Based Tool for Identification of Acute Aortic Dissection at Initial Presentation. Circulation 2011;123(20):2213-2218.
- Sutherland A, Escano J, Coon TP. D-dimer as the Sole Screening Test for Acute Aortic Dissection: A Review of the Literature." Ann Emerg Med 2008;52(4):339-343.


