A 26-year-old Spanish-speaking female patient presents to the emergency department (ED) with right-sided weakness after a witnessed seizure. The patient is postictal, combative, and has right-sided neglect. The patient's husband reports that she had been complaining of headaches and subjective fevers for the past day. Vital signs are as follows: Heart rate 167 beats per minute, blood pressure 119/80 mmHg, respiratory rate 38, oxygen saturation 95%, temperature 37 Celsius. Laboratory studies are remarkable for a glucose of 129, a negative urine pregnancy test, a negative toxicology screen, and a lactic acid of 5.4. HIV screening test ordered in the ED is positive. Chest radiograph shows bilateral lung infiltrates. Computed tomography (CT) reveals cerebral edema and a ring enhancing lesion in the left parietal lobe, consistent with toxoplasmosis (Figure 1).
Background
Toxoplasmosis is an infection caused by the single cell parasite Toxoplasma gondii. It is typically acquired through ingestion of oocysts, usually from soil or cat litter contaminated with feline feces. It can also be acquired via undercooked meat from an infected animal. In the United States, it is estimated that 11 percent of people aged 6 to 49 are seropositive for T. gondii, although the vast majority are completely asymptomatic.2 In comparison, toxoplasmosis of the CNS occurs in up to 40 percent of all patients with AIDS, and it is the most common opportunistic infection to cause encephalitis or focal intracerebral lesions.1 It is most commonly associated with a CD4 count of <100 cells/mm3.
CNS toxoplasmosis in the immunocompromised host can present in multiple ways. Frequently, the earliest symptoms are vague and may emerge as a minor headache or fever. More serious complications such as seizure, hemiparesis, aphasia, ataxia and even cranial nerve palsies, may develop.3 These serious complications are often the impetus for seeking immediate medical evaluation. While CNS toxoplasmosis in HIV positive patients is quite common, the differential must include brain abscess (fungal, parasitic, or bacterial), neoplasm, progressive multifocal leukoencephalopathy (PML), mycobacterial infection, viral encephalitis (CMV, HSV, etc), and stroke.4
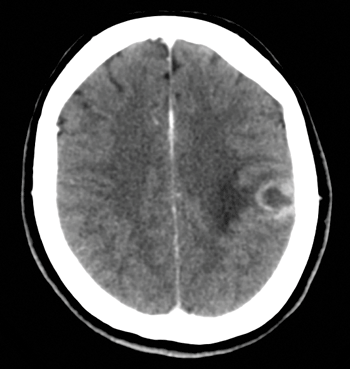 FIGURE 1. CT scan revealing cerebral edema and ring enhancing lesion in the left parietal region.
FIGURE 1. CT scan revealing cerebral edema and ring enhancing lesion in the left parietal region.
Diagnosis
Proper diagnosis requires a corresponding clinical syndrome in the setting of a CT or MRI that shows ring enhancing lesions.5 Serologic testing is also often used to clinch the diagnosis. The vast majority of patients with CNS toxoplasmosis are seropositive for anti-toxoplasma IgG antibodies. However, a small portion of these will not be positive. In these patients, a biopsy may be needed to provide definitive diagnosis.1
Although lumbar puncture (LP) is not required for diagnosis, it is recommended to evaluate for possible co-morbidities in the immunocompromised patient, or to confirm diagnosis in a patient whose IgG serum antibodies are negative. LP should be deferred in those cases wherein lies concern for herniation secondary to elevated intracranial pressure.
Treatment
Treatment of CNS toxoplasmosis is relatively straightforward. If the patient is critically ill, resuscitation and stabilization is paramount (secure airway, halt seizure activity, treat suspected sepsis, etc.). Specific treatment after onset of neurologic symptoms includes a combination of pyrimethamine, folinic acid, and sulfadiazine. Trimethoprim-sulfamethoxazole may be used as an alternative regimen. For those allergic to sulfa type medications, clindamycin may be substituted for sulfadiazine. Primary treatment continues for about 6 weeks and is followed by long-term suppressive therapy until CD4 counts are persistently >200 cells/mm.3 Meanwhile, the patient should either be started on or maintained on highly active antiretroviral therapy (HAART).3,4
For those patients presenting with seizure, treatment with antiepileptic drugs (AEDs) is an important consideration. Duration of treatment with AEDs generally lasts 3-6 months after initial presentation, but can be prolonged if chronic seizures develop. In choosing the appropriate AED, the goal is to limit the interaction with HAART medications. Older generations of AEDs tend to induce enzymes that decrease the efficacy of HAART. Newer AEDs, such as levetiracetam, have limited medication interactions, lower side effect profiles, and lower probability of toxicity.6,7 Seizure prophylaxis is not needed in HIV positive patients with T. gondii coinfection if the patient has not had prior CNS involvement.3
Case Conclusion
The patient was admitted to the intensive care unit for two days and was started on trimethoprim-sulfamethoxazole, HAART therapy, and an oral anti-epileptic drug. Serology was positive for IgG toxoplasma antibodies. CSF was negative for neurocysticercosis antibodies and mycobacteria. Sputum samples were positive for Mycobacterium avium complex. She was ultimately discharged from the hospital in good condition and continues to do well on her current regimen.
References
- Porter, SB, Sande, MA. Toxoplasmosis of the Central Nervous System in the Acquired Immunodeficiency Syndrome. New Engl J Med. 1992;327(23):1643-48.
- Grant IH, Gold JW, Rosenblum M, Niedzwiecki D, Armstrong D. Toxoplasma gondii serology in HIV-infected patients: the development of central nervous system toxoplasmosis in AIDS. AIDS. 1990;(6):519-21.
- http://www.cdc.gov/parasites/toxoplasmosis/disease.html. Accessed June 1, 2016.
- Dedicoat M, Livesley N. Management of toxoplasmic encephalitis in HIV-infected adults (with an emphasis on resource-poor settings). Cochrane Database Syst Rev. 2006. 3:CD005420.
- Kaplan JE, Benson C, Holmes KH, Brooks JT, Pau A, Masur H. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep. 2009;58:1-207.
- Siddiq, O, Birbeck, GL. Safe Treatment of Seizures in the Setting of HIV/AIDS. Curr Treat Options Neurol. 2013;15(4)529-543.
- Kirmani, BF, Mungall-Robinson, D. Role of anticonvulsants in the management of AIDS Related Seizures. Front. Neurol. 5:10.