Noninvasive positive pressure ventilation (NPPV) is the delivery of ventilatory support and positive pressure into the lungs without the need for an invasive endotracheal or tracheostomy tube.
How Does it Work?
During a normal breath cycle, a person’s diaphragm is pulled downwards to allow for lung expansion. This causes a decrease in intrathoracic pressure, allowing air to fill the lungs. When a patient is in respiratory failure, NPPV increases mean airway pressure, relieves dynamic hyperinflation, improves work of breathing, and in certain patient populations, decreases need for invasive mechanical ventilation and mortality. Additionally, NPPV decreases left and right ventricular preload and left ventricular afterload, making it an ideal therapy for cardiogenic pulmonary edema causing respiratory failure. Ultimately, the role of noninvasive support is to help reduce the patient’s work of breathing to avoid exhaustion from overworking the diaphragm as well as to improve oxygenation and ventilation. Appropriate patient selection is critical, as inappropriate use of NPPV may delay time to intubation and worsen patient outcomes.
Indications
|
Condition |
Level of evidence for NPPV use |
|
Chronic Obstructive Pulmonary Disease (COPD) exacerbation with acute hypercarbia1
Cardiogenic pulmonary edema2,3
|
Strong recommendation |
|
Asthma exacerbation
Immunocompromised patients with respiratory failure
De novo acute respiratory failure - Hypoxemic respiratory failure in patients without chronic cardiopulmonary disease - Ex. pneumonia, ARDS
Chest wall trauma |
May benefit some patients |
|
Preoxygenation for intubation
Weaning from mechanical ventilation
Patients with high risk of extubation failure after successfully weaning off of invasive mechanical ventilation (patients with COPD and post-surgery in particular)
Palliative support for work of breathing in patients who have chosen to be do not intubate (DNI) |
Less commonly used, but some evidence exists supporting use |
Absolute Contraindications to NPPV
- Patients with respiratory or cardiac arrest
- Patient with inability to fit mask (morbid obesity, extensive trauma, burns involving the face)
- Need for emergent invasive mechanical ventilation
Relative Contraindications to NPPV
- Extreme agitation despite treatment with medications
- Inability to protect airway (cough or swallowing impairment)
- Facial bone/basilar skull fracture
- Recent gastrointestinal (GI) hemorrhage
- Untreated pneumothorax
Bilevel Positive Airway Pressure (BiPAP)
In this mode, breaths are triggered by the patient unless apneic, in which the backup rate is responsible for initiation of breaths. As its name suggests, this mode delivers two different pressures: inspiratory positive airway pressure (IPAP) and expiratory positive airway pressure (EPAP). Inspiration is an active process that requires more energy compared to expiration, which is a passive process, therefore the pressure applied in IPAP is always greater than EPAP.
IPAP is the pressure that assists with helping a person inhale. It reduces the work a person must do to inhale by offloading the diaphragm and other muscles involved in respiration, relieves dynamic hyperinflation, and overall decreases work of breathing. EPAP increases oxygenation via recruitment of collapsed alveoli and is analogous to positive end-expiratory pressure (PEEP) on a mechanical ventilator. This is most useful in patients with alveolar collapse (eg, atelectasis, pulmonary edema, etc.) or pulmonary edema.
The hemodynamic effects of EPAP are analogous to PEEP on the ventilator: It decreases right and left ventricular preload and left ventricle afterload which can help with forward flow of blood in the heart.2 Importantly, EPAP increases right ventricular afterload, so this may have deleterious effects in patients with significant pulmonary hypertension.
How to Titrate Your BiPAP
The 4 settings that must be set are:
- Fraction of Inspired Oxygen (FiO2)
- EPAP
- IPAP
- Respiratory Rate (RR)
First, decide: Is this an oxygenation or a ventilation issue?
To improve oxygen: Titrate your FiO2 and EPAP
- This should be adjusted for a goal saturation of approximately 92-98% in otherwise healthy patients and 88-92% in patients with chronic hypercapnic conditions.4
- Remember EPAP = PEEP
To improve ventilation: Titrate your Driving Pressure and Respiratory Rate
- Driving Pressure = IPAP - EPAP
- The difference between IPAP and EPAP is known as driving pressure, which directly correlates to tidal volume, which is defined as the amount of air that moves in or out of the lungs during a normal breath.
- This is approximately 500 mL in an average adult, although tidal volume can vary greatly based on ideal body weight; effort should be made to titrate based on appropriate tidal volume whenever possible.
- The driving pressure should be titrated so the patient can achieve an adequate tidal volume and minute ventilation on the BiPAP monitor.
- Respiratory rate is set as a back-up, typically around 12. Ideally the patient continues to breathe spontaneously and triggers IPAP/EPAP by spontaneous effort.
- If they experience a period of apnea, then the machine will trigger the minimum set respiratory rate.7 Use with extreme caution in patients approaching apnea. The backup respiratory rate is the equivalent of bagging the patient if the patient becomes apneic!
Other settings to consider:
- I-Time = Inspiratory Time. Decreasing the inspiratory time will allow for more time to exhale, thus decreasing the I:E ratio (1:3-1:4). Consider decreasing your I-Time in the obstructed patient (such as COPD) to allow more time for exhalation and reduce breath stacking.
- Rise time is the speed at which inspiratory pressure increases to the set target IPAP. A shorter rise time allows for faster inhalation, thus decreasing your I-Time and decreasing your I:E ratio.
To determine whether your current BiPAP settings are adequate, there are a few things clinically you should assess at bedside once the mask is applied:
Is there adequate oxygenation on pulse oximetry?
- Pulse oximetry with an adequate waveform is adequate and often superior to serial ABGs.
Does your patient overall look more comfortable breathing?
- Do they still have signs of respiratory distress (eg, tachypnea, diaphoresis, retractions, tripoding, decreased mental status, etc.)?
Look at the BiPAP machine monitor: Is the tidal volume adequate?
- Aim for ~6-8cc/kg ideal body weight
There is no universal approach to titrating BiPAP settings. The best titration strategy is to pick a setting and re-assess patient’s comfort and tidal volumes at bedside. Remember, the goal of BiPAP is to make the patient in respiratory distress more comfortable, not to fix the numbers of an arterial blood gas (ABG) as fast as possible. Do not forget to frequently re-assess your patients for any deterioration, as delays in intubation are consistently associated with worse outcomes.
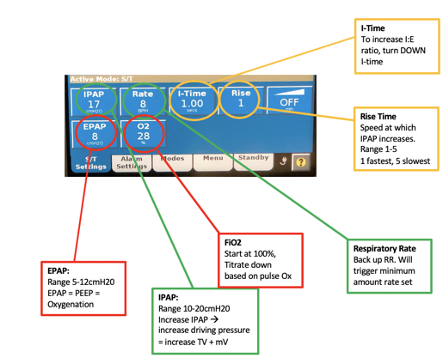
Figure 1: BiPAP machine interface
Continuous Positive Airway Pressure (CPAP)
This is a setting where airflow is introduced into the airway to maintain a continuous pressure to stent the airways open throughout a spontaneous breathing cycle. This essentially is continuously delivering PEEP. CPAP differs from BiPAP because it delivers a constant pressure throughout the respiratory cycle, during both inspiration and expiration. This mode is preferred for disease states requiring oxygenation, as it does not assist with ventilation because it does not assist with inspiration. This works to improve oxygenation by increasing mean airway pressure thus decreasing atelectasis and increasing surface area of alveoli to improve V/Q matching and decreasing preload and afterload in patients with cardiogenic pulmonary edema.1
Average Volume Assured Pressure Support (AVAPs)
This is a relatively newer modality that combines both volume and pressure-controlled non-invasive ventilation. Rather than having one fixed IPAP setting, this mode sets a minimum and maximum value of IPAP. The tidal volume is then preset, allowing the ventilator to adjust the inspiratory pressure from breath to breath to ensure the preset tidal volume is delivered. This decreases patient-ventilator asynchronization as the inspiratory pressure changes with each breath, thus improving patient comfort.3
Pitfalls
- Delaying tracheal intubation
- Failing to frequently reassess patient after initiation of NPPV
- Applying NPPV in patients who do not benefit from it
- Following blood gas results rather than overall clinical picture
- Forgetting potential hemodynamic consequences of NPPV: hypotension particularly if EPAP or CPAP is high and increased right ventricular afterload in patients with RV failure
|
|
Overview |
Common Initial Settings |
Common Indications |
|
CPAP |
Continuous pressure delivered. Assists with oxygenation, NOT ventilation. |
CPAP 5 FiO2 100% |
Type 1 hypoxemic respiratory failure due to cardiogenic pulmonary edema
|
|
BiPAP S/T - spontaneous/ timed |
IPAP and EPAP is set to create a driving pressure that assists in ventilation in addition to oxygenation |
IPAP 10 EPAP 5 FiO2 100% RR 12 |
Type 2 hypercapnic respiratory failure OR mixed Type 1 & respiratory muscle weakness |
|
AVAPS |
Hybrid mode where inspiratory pressure is automatically adjusted to delivered preset tidal volume |
Max P: 20 Min P: EPAP + 4 EPAP 5 Vt 400-600 mL FiO2 100% RR 12 |
Type 2 hypercapnic respiratory failure9 - Can improve patient compliance if patient is not tolerating BiPAP |
Acknowledgment
The authoring team wishes to offer special thanks to faculty reviewer Gabriel Wardi, MD, MPH, Associate Professor of Clinical Emergency Medicine and Medicine, Department of Emergency Medicine, Division of Pulmonary Critical Care and Sleep Medicine, University of California, San Diego
PATIENT-FOCUSED RESOURCE
The National Council on Aging offers a practical tip sheet to help patients understand how to clean their CPAP machines at home.
"How to Clean a CPAP Machine"13 can be read online or downloaded for print here: https://www.ncoa.org/adviser/sleep/how-clean-cpap-machine/.
References
- Lightowler JV, Wedzicha JA, Elliott MW, Ram FSF. Non-invasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysis. BMJ. 2003;326(7382):185.
- Gray A, Goodacre S, Newby DE, Masson M, Sampson F, Nicholl J; 3CPO Trialists. Noninvasive ventilation in acute cardiogenic pulmonary edema. N Engl J Med. 2008;359(2):142-151.
- Cabrini L, Landoni G, Oriani A, et al. Noninvasive ventilation and survival in acute care settings: a comprehensive systematic review and meta-analysis of randomized controlled trials. Crit Care Med. 2015;43(4):880-888.
- Pinto VL, Sharma S. Continuous Positive Airway Pressure. [Updated 2022 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482178/.
- Margutti E, Greco I, Brambilla AM, et al. Non-invasive ventilation in acute respiratory failure: the key “W” questions. Intern Emerg Med. 2017;12:1307-1311.
- Yarrarapu SNS, Saunders H, Sanghavi D. Average Volume-Assured Pressure Support. [Updated 2022 Sep 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560600/.
- Weekley MS, Bland LE. Oxygen Administration. [Updated 2022 Apr 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551617/.
- Agarwal R, Aggarwal AN, Gupta D, et al. Non-invasive ventilation in acute cardiogenic pulmonary oedema. Postgrad Med J. 2005;81(960):637-643.
- Pooboni S. Noninvasive Ventilation Procedures. Medscape. Updated July 18, 2022.
- Britt D. CE Article: BiPAP Essentials for Prehospital Providers. EMS World. August 2017.
- Scala R, Pisani L. Noninvasive ventilation in acute respiratory failure: which recipe for success? Eur Respir Rev. 2018;27:180029.
- Yarrarapu SNS, Saunders H, Sanghavi D. Average Volume-Assured Pressure Support. [Updated 2022 Sep 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560600/.
- Smith K, Lyda EU, Currie D. How to Clean a CPAP Machine. NCOA Adviser. Oct. 24, 2023. Available at https://www.ncoa.org/adviser/sleep/how-clean-cpap-machine/.



