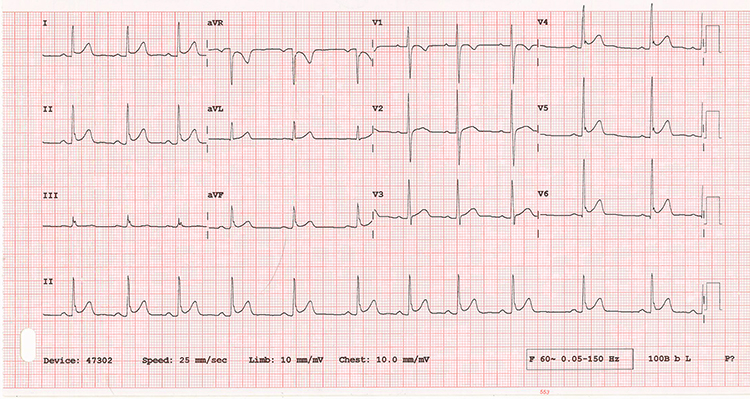
A 22-year-old female presents with chest pain. What's your interpretation of the resulting EKG?
ANSWER
The ECG shows a sinus rhythm at 70 bpm with a normal axis and normal intervals. There are STE >1 mm in leads I, II, aVF, V4-V6 and STD >1 mm in aVR with no other reciprocal changes. This distribution of ST segment changes is not consistent with an expected anatomic distribution of a coronary artery and suggests a non-ACS etiology.
The differential for non-ACS causes of STE is broad and includes conduction abnormalities (eg, LBBB, pre-excitation syndromes), structural abnormalities (LVH, LV aneurysm), and metabolic abnormalities (eg, hyperkalemia). This ECG is consistent with Early Repolarization, commonly referred to as Benign Early Repolarization (which may be a misnomer as current research suggests this may be associated with an increased incidence of arrhythmic sudden cardiac arrest).
The terms Normal Variant ST Elevation and Normal Variant Early Repolarization are typically used to refer to isolate STE in V1-V4. Given this patient’s age, chief complaint, and diffuse distribution of STE without non-aVR reciprocal changes, pericarditis should also be considered.
To distinguish between pericarditis and BER, compare the J point elevation to the T-wave amplitude in V6. A ratio of < 0.25, as seen in the case ECG, suggests BER. The other “classic” finding in this ECG that suggest BER is the “fishhook” or notching pattern at the J point in leads V4-V6. The other ECG findings associated with BER and pericarditis are listed in the Learning Points.
After a thorough history and examination, a chest x-ray was performed, which was normal, and patient was discharged home with ibuprofen for suspected musculoskeletal chest pain. She later presented to another ED where she underwent CTA imaging, bilateral leg ultrasounds, and serial troponin testing, all to no avail.
LEARNING POINTS
2013 ACCF/AHA ECG Criteria for Acute Myocardial Infarction
- New, or presumed new, STE at the J point in ≥2 anatomically contiguous leads .
- ST-segment is measured from the isoelectric baseline, typically the TP segment
- ≥ 1 mm in all leads other than V2-V3 . ≥ 1.5 mm in women in V2-V3
- ≥ 2 mm in men in V2-V3 (2013 guidelines simplified V2-V3 cutoffs in men from 2012 guidelines)
- ≥ 0.5 mm in V7, V8, or V9 (posterior leads) in posterior MI
- Absence of LVH, LBBB, or paced rhythm
- New LBBB is no longer considered a STEMI equivalent
- STE < 1 mm in a clinically suggestive presentation should prompt concern for STEMI
Benign Early Repolarization
- Widespread concave STE, most often in V1-V4 (can include II, II, aVF, V5 and V6)
- “Fishook” or notching pattern, typically in V4
- QRS to T-wave concordance
- Asymmetric T-waves (descending limb steeper than ascending limb)
- No reciprocal ST-segment changes (except in aVR)
- Normal R-wave progression
- ECG stability over time
- Found most often in younger patients
Pericarditis
- 4 stages of transient ST and PR segment changes
- EKG features (stage 1)
- Concave upward STE typically 2-4 mm
- STE and PR-segment depressions diffusely in all leads except aVR and V1
- Prominent T waves
- Spodick’s sign (down sloping TP segment)
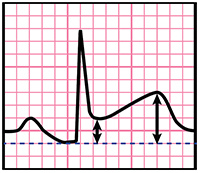 To distinguish between pericarditis and BER, compare J point elevation to T-wave amplitude in V6 (see image)
To distinguish between pericarditis and BER, compare J point elevation to T-wave amplitude in V6 (see image)
- Ratio ≥ 0.25 suggests pericarditis
- Ratio < 0.25 suggest BER
For more on BER and pericarditis, please see pages 1, 2, and 7-10 of the EMRA EKG Guide.
Editor’s Note: I received some feedback from my close friend and fellow EKG aficionado Dr. Joe Polinksi on the ECG Challenge from the April/May issue of EM Resident. He pointed out that the last sentence of the 1st paragraph states the treatment options for stable irregular WCT include amiodarone, which is not an ideal choice if there is suspected underlying WPW, as amiodarone has nodal blocking properties and questionable efficacy on increasing the refractoriness of the accessory pathway. Of note, section 8.1.3.1.6 of the ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation states “In hemodynamically stable patients with [Afib and] preexcitation, type I antiarrhythmic agents or amiodarone may be administered intravenously.” This recommendation was not changed in the 2011 Focused Update of the 2006 Guidelines. The take-home point is that procainamide or cardioversion are the safest treatment options for hemodynamically stable irregular WCT with suspected WPW.



