Ultrasound in the emergency department can reveal the echogenicity of the renal pyramids in Medullary Sponge Kidney. Despite previous episodes and presentations, it is often undiagnosed or overlooked by physicians, and chronic presentations can cause diagnostic dilemmas for emergency physicians.
Case
A 31-year-old female with a history of nephrolithiasis and hematuria presented to the emergency department with a chief complaint of right flank pain and hematuria for the past three days, unrelieved by over the counter ibuprofen or acetaminophen. The patient reported pain, which was dull and constant in nature, which fluctuated to a sharper pain associated with movement. The pain was localized to the right flank, with radiation to the right lower pelvis.
Investigation of the abdomen, pelvis and kidneys with an ultrasound was unremarkable, except for bilateral renal echogenicity. Focused renal examination of the right kidney measured a size of 9.5x5.2x3.7 cm (Figure 1, 2) and 10x3.5x4.4 cm of the left, and was negative for hydronephrosis or focal masses, bilaterally. The right kidney was marked with a 5 mm stone in the lower pole, without focal masses. There were no stones in the left kidney. On careful inspection, diffuse increased echogenicity of the renal pyramids was visualized bilaterally.

Figure 1: Ultrasound investigation of the right and left right kidney in 2D long views, reveal diffuse echogenicity seen here. The right kidney measured a size of 9.5x5.2x3.7 cm, whereas the left kidney measured a size of 10x3.5x4.4 cm. The right kidney was further marked with a 5 mm stone in the lower pole.
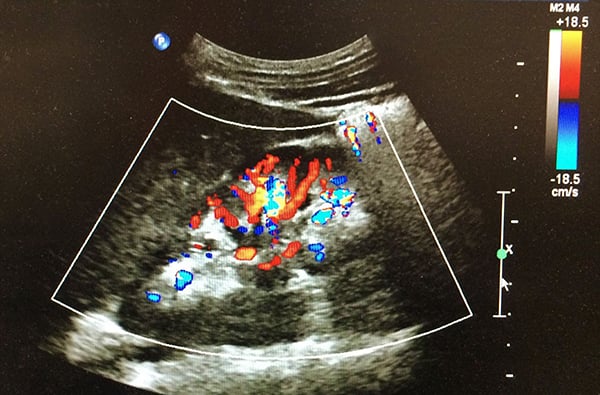
Figure 2: Ultrasound investigation of the right and left kidney in a 2D long view doppler flow. Diffuse echogenicity is seen.
The patient was given Toradol IV with improvement of pain. The patient also received IV fluid hydration to aid in calcium stone management. Labs were drawn and results remained with normal limits. The patient indicated she had approximately five previous episodes of similar pain over the years. However, these episodes did not require hospital admission. The diagnosis of medullary sponge kidney was made from assessment of the case and medical history, and discussion with the patient for management with oral hydration at home as well as pain management was recommended. The patient was discharged approximately five hours after presentation.
Discussion
Medullary Sponge Kidney (MSK), also known as Cacchi-Ricci disease, is an uncommon and benign congenital disorder affecting less than 1% of the population1 and is thought to be attributed to the developmental abnormality between the ureteral-bud and the metanephric blastema in utero.2 Nonetheless, investigations for the proteomic biomarkers responsible for the defects or genetic transmission is limited, and patients will often present with a negative family history and phenotype. As medical referrals and consults for MSK are increasing at a rate out of proportion to the prevalence of the disease,3 understanding MSK in the emergency department (ED) can allow for appropriate patient care and management. Further, although the renal pathogenesis of MSK is associated with Beckwith-Widemann syndrome and renal hemihypertrophy, it is important to differentiate MSK from polycystic kidney disease and tubulointerstitial kidney disease as these can present with similar imaging results despite the unrelated pathophysiology.4
MSK is often asymptomatic. However, clinical presentation is often among adult women between 30 to 50 years of age does demonstrate a history of recurrent painless hematuria, increased frequency of urinary tract infections, and recurrent calcium stones.5-7 As there is no gold standard for the diagnosis of MSK, emergency physicians in the ED can use ultrasound for renal vascular flow analysis to visualize the renal architecture for the dilation of the terminal collecting ducts and/or diffuse medullary cysts, as was done in the management of this case. Other imaging studies include a preference of non-contrast computed tomography scan, as well as intravenous pyelography though rarely used, and magnetic resonance imaging with gadolinium.3 Although ultrasound is less specific than other imaging modalities, it’s benefits with time and cost effectiveness make it a favorable imaging candidate, which can reliably show a uniform echogenicity of the corticomedullary junction and hydronephrosis due to stone obstruction, seen in MSK.8
Initial treatment of MSK involves hydration for calcium stones, as well as the management of sequela (UTI, pain). Thorough case investigation with patient history further allows for cost-effective management and patient education. As seen in this case, effective management and awareness of this benign disease resulted in a favorable outcome.
Take-Home Points
-
Patients with a recurrent history of nephrolithiasis and hematuria may have undiagnosed medullary sponge kidney. Although a benign disease, the management of sequela associated with MSK, such as antibiotics for urinary tract infections, and analgesics for pain management, is recommended.
-
The awareness and understanding of the pathophysiology and presentation of MSK in the ED, where ultrasound imaging is frequently used for screening and diagnostic purposes, is valuable in establishing a management plan consisting of a diagnostic work up, potential medical consults and other invasive investigations.
-
Patient education to understand the pathogenesis of MSK can alleviate anxiety and frustration and can allow for cost effective management.
References
1. Palubinskas AJ. Renal Pyramidal Structure Opacification in Excretory Urography and its relation to Medullary Sponge Kidney. Radiology. 1963;81:963-970.
2. Gambaro G, Feltrin GP, Lupo A, et al. Medullary sponge kidney (Lenarduzzi–Cacchi–Ricci disease): A Padua Medical School discovery in the 1930s. Kidney Int. 2006;69(4):663-670.
3. Borofsky M. The Diagnostic Dilemma of Medullary Sponge Kidney. University of Chicago. Available at: https://kidneystones.uchicago.edu/the-diagnostic-dilemma-of-medullary-sponge-kidney/ Accessed: August 21, 2019.
4. Goldfarb DS. Medullary sponge kidney. Uptodate. Available at: https://www.uptodate.com/contents/medullary-sponge-kidney?search=Medullary%20Sponge%20Kidney&source=search_result&selectedTitle=1~38&usage_type=default&display_rank=1 Accessed: August 21, 2019.
5. Parks JH, Coe FL, Strauss AL. Calcium nephrolithiasis and medullary sponge kidney in women. N Engl J Med. 1982;306(18):10881091.
6. Yagisawa T, Kobayashi C, Hayashi T, Yoshida A, Toma H. Contributory metabolic factors in the development of nephrolithiasis in patients with medullary sponge kidney. Am J Kidney Dis. 2001;37(6):1140-1143.
7. Ghosh AK. Medullary sponge kidney. Medscape Available at: https://emedicine.medscape.com/article/242886-overview Accessed September 12, 2014.
8. Levine E, Hartman DS, Meilstrup JW, et al. Current concepts and controversies in imaging of renal cystic diseases. Urol Clin North Am. 1997;24(3):523-543.


