Since the dawn of time, biological life has been affected by the extremes of temperature. Militarily, wars have been won and lost due to the devastation brought on by hypothermia. Hannibal lost nearly half his men in the Second Punic War. Napoleon's army was crippled in the harsh winter of Russia in 1812. Arguably the greatest American generation suffered through the infamous European winters of WWII.
Unfortunately, accidental hypothermia remains a substantial cause of death in our developed nation with nearly 1500 people dying yearly. In 1999, a Swedish physician suffered from one of the lowest recorded hypothermia cases, with a core temperature of 13.7°C after 9 hours of resuscitation - including initiating of ECMO.
Pathophysiology
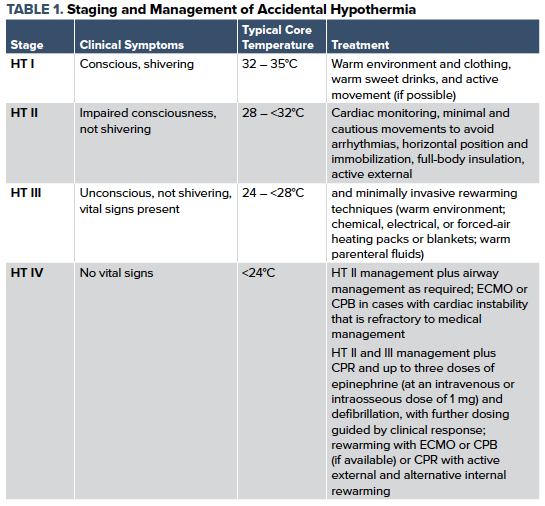
Accidental hypothermia refers to an involuntary drop in the body’s core temperature below 35°C (95°F). As the body cools with cold exposure, there is a natural response to maintain a normal core temperature, with involuntary shivering and active movement. The ability to regulate temperature and respond appropriately is multifactorial depending on age, exposure, health, nutrition, medications, and intoxicating substances. In the urban setting, the majority of patients presenting with accidental hypothermia are the homeless and alcoholics. Other at-risk populations include the extremes of age, who have a weakened ability to thermoregulate.
Clinical Manifestations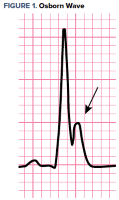 Cold exposure can lead to an incredibly variable clinical presentation. As the body temperature begins to decrease - breathing, circulation, and level of consciousness are affected. Below 95°F, patients will begin to have decreased cognitive function and difficulty with fine motor dexterity. Hypertension and tachycardia quickly progress to cardiac instability with associated hypotension, bradycardia, and ultimately dysrhythmia. EKG findings can consist of bradycardia, QRS widening, prolonged PR and QT intervals, as well as the classic Osborn wave.
Cold exposure can lead to an incredibly variable clinical presentation. As the body temperature begins to decrease - breathing, circulation, and level of consciousness are affected. Below 95°F, patients will begin to have decreased cognitive function and difficulty with fine motor dexterity. Hypertension and tachycardia quickly progress to cardiac instability with associated hypotension, bradycardia, and ultimately dysrhythmia. EKG findings can consist of bradycardia, QRS widening, prolonged PR and QT intervals, as well as the classic Osborn wave.
Respiratory status may become tenuous as the initial tachypnea settles and eventually leads to respiratory depression as core temperature continues to drop. Pulmonary edema and aspiration pneumonia are common findings in the profoundly hypothermic patient.
Prehospital Management
The prehospital management of a suspected hypothermic patient can be broken down to careful movement, basic and advanced life support, passive and active rewarming, and transportation to an appropriate center. There is a concept known as Rescue Collapse, which refers to the cardiac instability that is caused by the sheer movement of a patient suffering from severe hypothermia. Even basic movements can cause ventricular disturbance leading to fatal arrhythmia.
Emergency Department Management
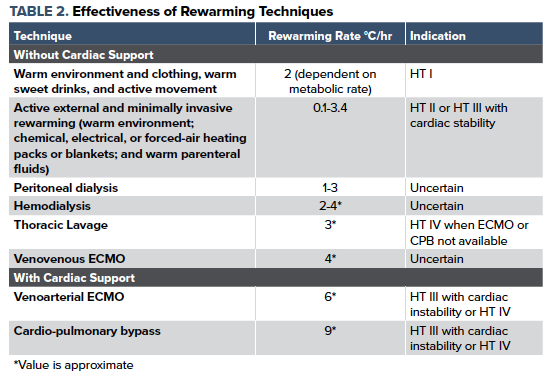
Determining an accurate core body temperature can often be difficult but remains paramount in the management of the hypothermic patient. An esophageal probe is a preferred method in your intubated patients. This is closely followed by the bladder probe. If unable to obtain an esophageal or bladder temperature, then rectal temperature becomes the ideal method. Modified advanced life support should be initiated as soon as possible, with the first and foremost focus remaining on rewarming the patient. Pharmacologic interventions, such as epinephrine and other vasoactive agents, can be arrhythmogenic while having little to no effect, and thus should generally be avoided. Most arrhythmias convert spontaneously into normal sinus rhythm during rewarming. Defibrillation can be attempted if necessary but is typically unsuccessful until the core temperature is above 28-30°C. If defibrillation is unsuccessful, then further attempts should be delayed until the temperature is above 30°C. Transvenous pacing is considered hazardous for hypothermia-induced bradydysrhythmias.
Serum potassium levels have been a controversial marker of non-survival. Research has suggested that serum potassium greater than 12 mmol per liter (10 mmol per liter in some institutions) may be used as a hard stop for whether or not CPR may provide benefit. There is no consensus on how hyperkalemia is best treated in levels less than 12mmol per liter in the non-cardiac arrest patient.
Disposition
The disposition of the patient is highly variable depending on the degree of hypothermia and response to therapies administered. Patients who are classified as mild to moderate may be briefly observed in the emergency department and discharged home if they have an appropriate response to management with good social support. Patients who are classified as moderate to severe, or those requiring invasive procedures, should be admitted to the hospital for further evaluation and observation. Transfer to an ECMO capable facility should be considered for any patient with cardiac instability, dysrhythmia, or severe hypothermia unresponsive to otherwise maximal invasive therapies. Termination of resuscitative efforts generally isn’t considered until the core temperature as reached 32°C without other markers of futility, ie, trauma incompatible with life or a potassium >12mmol).
Conclusion
Patients suffering from accidental hypothermia should be managed aggressively. Those without cardiac instability can be managed with active, external warming and minimally invasive warming techniques. Patients with severe hypothermia, especially those in cardiac arrest, should be treated at a facility capable of extracorporeal rewarming. Given the advancements in rewarming techniques, the prognosis for patients suffering from hypothermia has improved. For patients who suffered cardiac arrest secondary to primary hypothermia and were subsequently placed on ECMO, neurologically intact survival is as high as 50%; while nearly 100% of all other hypothermic patients have full neurologic recovery.
References
- Brown DJ, Brugger H, Boyd J, Paal P. Accidental hypothermia. New England Journal of Medicine. 2012 Nov 15;367(20):1930-8. PMID:23150960
- Truhlář A, Deakin CD, Soar J, Khalifa GE, Alfonzo A, Bierens JJ, Brattebø G, Brugger H, Dunning J, Hunyadi-Antičević S, Koster RW. European Resuscitation Council Guidelines for Resuscitation 2015: Section 4. Cardiac arrest in special circumstances. Resuscitation. 2015 Oct;95:148. PMID: 26477412
- Dunne B, Christou E, Duff O, Merry C. Extracorporeal-assisted rewarming in the management of accidental deep hypothermic cardiac arrest: a systematic review of the literature. Heart, Lung and Circulation. 2014 Nov 1;23(11):1029-35. PMID: 25043580
- Baumgartner EA, Belson M, Rubin C, Patel M. Hypothermia and other cold-related morbidity emergency department visits: United States, 1995–2004. Wilderness & environmental medicine. 2008 Dec 1;19(4):233-7. PMID: 19099327
- Schaller M, Fischer A, Perret C. Hyperkalemia. A prognostic factor during acute severe hypothermia. JAMA. 1990;264(14):1842-1845.
- Cline DM, Ma OJ, Meckler GD, Tintinalli JE, Stapczynski JS, Yealy D, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8th Edition. McGraw-Hill Education / Medical; 2015.
- Swaminathan A. "Accidental Hypothermia", REBEL EM blog, October 8, 2018. Available at: https://rebelem.com/accidental-hypothermia/



