The management of removal of foreign objects from the extremities and phalanges is essential in emergency medicine management; in particular, understanding of the mechanism of injury and details about the object impaled is important.
Case
A 68-year-old right-hand dominant male with a past medical history of hypertension, type 2 diabetes mellitus presented to the ED after sustaining a nail gun penetrating trauma to the left thumb. The patient reported that approximately 3 hours prior to arrival to the ED, he was using a nail gun to work on a home renovation project when he accidentally impaled himself with the nail gun in his left thumb. The patient felt immediate pain at the left thumb and was unable to pull the nail out of his digit himself. He reported adequate hemostasis with a soft dressing applied to the site of injury. He sought help at a local urgent care prior to arrival to the ED, stating that they were unsuccessful in removal of the impaled nail. He reported that the nail was a threaded nail, and not a simple screw. The patient reported he was up to date on his tetanus vaccination and had a booster administered within the year. He denied any new onset paresthesias, numbness, or tingling into the distal aspect of the left thumb. The patient reported no use of anticoagulants. He denied history of injury, trauma, or prior surgeries to the left thumb.
On physical exam, he was in no acute distress, resting comfortably sitting upright in an ER chair having ambulated well into the ED. He was vitally and hemodynamically stable. Focused exam of his left thumb was significant for an adequately perfused digit that was warm, with capillary refill <2 seconds with palpable radial and ulnar pulses. Sensation was intact to the distal most aspect of the left thumb with intact 2-point discrimination to <5mm. His left thumb had a large threaded metal nail, measuring approximately 7.5cm in length and 3.2mm wide, protruding from the distal aspect of the digit. He was unable to demonstrate the ability to actively flex at the interphalangeal joint of the thumb. Pain was managed with Hydrocodone 5-325 mg in the ER, and he received prophylactic 2g IV Cefazolin antibiotic for soft tissue injury and bone penetration.





INVESTIGATION & MANAGEMENT
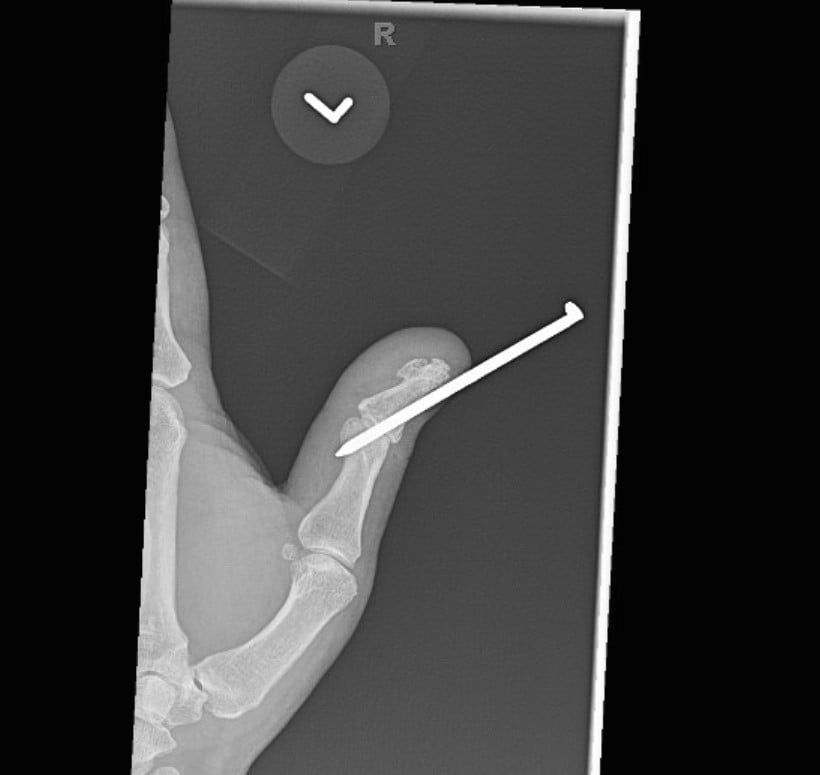
Radiographs were obtained including anterior-posterior and lateral views of the left thumb which demonstrated a penetrating injury of a metallic object (in this case, the threaded nail). The nail on X-ray did appear to pierce the base of the distal phalanx with extension through the interphalangeal joint into the thumb proximal phalanx with an associated vertically oriented split fracture of the proximal phalanx, evident with increased radiolucency on these films. No gas within the soft tissues or other identified foreign bodies; fractures, dislocation, or other acute bony abnormalities were noted. The hospital site has an orthopedic surgery residency program, and the orthopedic surgery resident was consulted given the bony involvement and the recommended outpatient management with an orthopedic hand surgeon.
The management of this case was bedside removal of the foreign metal nail. A Betadine scrub brush was used with sterile saline to copiously wash and irrigate the surrounding area of penetrating metallic nail. In sterile fashion, and using sterile pliers, the metallic nail was removed using counterclockwise rotation in order to disengage the nail from the penetrated bone. The wound was again copiously irrigated with sterile saline and scrubbed again with Betadine. The thumb was dressed using sterile Adaptic and bacitracin ointment. A left thumb spica cast was applied for immobilization of the digit and to maintain appropriate anatomic alignment. The patient tolerated the removal of the metallic nail, washouts and application of the cast well. He was neurovascularly intact following the treatment.


Post-foreign body removal with cast application X-rays were obtained which redemonstrated the vertically oriented, longitudinal fracture of the left thumb proximal phalanx extending into the interphalangeal joint. Removal of the foreign metal nail also allowed for appreciation of an intra-articular fracture at the distal ulnar aspect of the proximal phalanx where the metallic nail had been previously located, and a distal phalanx base fracture as well. No retained metallic foreign bodies were identified. Of note, there was no involvement of the metacarpal phalangeal joint of the thumb, making this an isolated injury involving only a single joint of the thumb.
Post procedure, he was neurovascularly intact following the removal of the metal nail and after application of thumb spica cast. He was discharged in stable condition from the emergency department with PO antibiotics of Cefalexin 500mg 4 times daily for 10 days and PRN pain management with acetaminophen and or ibuprofen as needed, including rest, ice, and elevation of the affected thumb. The patient was given thorough cast care instructions, including education about compartment syndrome, education for signs and symptoms of potential infection, and strict return precautions discussed.
DISCUSSION
The management of removal of foreign objects from the extremities and phalanges is essential in emergency medicine management; in particular, understanding of the mechanism of injury and details about the object impaled is important. In this case, fasteners such as nails and screws vary between driven-in with a hammered or direct force of motion, versus a rotational force, which is often used with screws. The metal nail described in this case was one with a spiral thread on the shank, beneficial for home renovation projects as it creates a thread-like interlock and increasing withdrawal capacity.1 Further, penetrating nail gun and screw injuries to the hand commonly occur in both professional and nonprofessional settings, where 14% of nail gun injuries that occur at home involve a hand or finger trauma.2
These injuries can be complicated if there is bony, tendinous, vascular, or joint involvement. However, most cases involve a retained nail or screw with injury to surrounding soft tissue. Extraction can be complicated by barbs or threads. In the instance of barbed or threaded nails, typically the head of the nail is removed and then extracted in the direction of entry.3 Furthermore, one case described an injury of a barbed nail penetrating the volar soft tissue completely through the distal phalanges of the second and third digits. On radiographic imaging there was no bony involvement identified, and no barbs were embedded in the soft tissue of the digits. In that case, the removal of the foreign body was performed in the operating room with fluoroscopy to confirm the absence of retained foreign bodies. Irrigation was performed with pulse lavage.4 A similar case presented involved a nail embedded deeply through the first, second, and third digits. The patient was neurologically and vascularly intact with no evidence of bony involvement and the nail was also removed in the operating room in retrograde fashion with confirmation of no retained foreign bodies via X-ray and finished with irrigation and left open.4
Another case discusses a barbed screw impaling the mid left palm in line with the third digit in close proximity to Kaplan’s line of the palmar arch. In this case, the barbs extended through the overlying lumbrical muscle and flexor tendon of the middle finger. Once again, no fractures were identified, but there was median nerve compression secondary to traumatic edema at the mid-carpal tunnel area. Open exploration was performed in the operating room and extraction under direct visualization followed by irrigation with sterile normal saline and then closed with sutures.5 Many of these cases have similar methods of extraction, but published literature describes a new method proposing tying a thick suture around the distal aspect of the nail, so as the nail is removed in retrograde fashion, the suture pulls through. Furthermore, this allows identification of the tract for directed debridement and irrigation.6
TAKE-HOME POINTS
Management of hand injuries due to nail guns further includes pain management, ensuring a Tetanus vaccination update if indicated and administering antibiotics, preferably with anti-staphylococcal and anti-pseudomonal coverage, both in the ED prophetically with the patient and continued outpatient.7,8 The case discussed here, similar to a previous study of hand injuries, presents an efficient method of extraction of a threaded screw in a patient digit with bony involvement that offers successful patient outcomes while efficiently avoiding extensive resources, including that of operating room costs, equipment, staffing, resources and patient cost and time.9
References
- Simpson Strong Tie website https://www.strongtie.com/products/fastening-systems/technical-notes/nails-overview
- Lipscomb HJ, Dement JM, Nolan J, et al. Nail gun injuries in residential carpentry: lessons from active injury surveillance. Inj Prev 2003;9(1):20-4.
- Hoffman DR, Jebson PJ, Steyers CM. Nail gun injuries of the hand. Am Fam Physician. 1997;56(6):1643-1646.
- Pierpont YN, Pappas-Politis E, Naidu DK, Salas RE, Johnson EL, Payne WG. Nail-gun injuries to the hand. Eplasty. 2008;8:e52.
- Lanteri A, Celestin R, Fleegler E. Barbed screw through the hand. Eplasty. 2012;12:ic3.
- Malahias M. Nail gun injuries: a simple method to facilitate exploration. Ann R Coll Surg Engl. 2008;90(6):523-524.
- Chintapalli P, Phoenix E, Cullen S, Dolan RT. Nail Gun Injuries to the Hand and Wrist: A Systematic Literature Review. Cureus. 2025 Feb 18;17(2):e79216.
- Pierpont YN, Pappas-Politis E, Naidu DK, Salas RE, Johnson EL, Payne WG. Nail-gun injuries to the hand. Eplasty. 2008;8:e52. Epub 2008 Nov 13. PMID: 19079574; PMCID: PMC2586285.
- Horne BR et al. Review of 88 nail gun injuries to the extremities. Injury, Volume 39, Issue 3, 357–361.



