Osteochondral defect (OCD), historically referred to as Osteochondritis Dissecans, was described by Dr. Franz König more than 125 years ago. Rarely seen in the ED, it should remain in your differential - missing this diagnosis can lead to early-onset osteoarthritis.
Case
An 18-year-old male presented to the ED with a chief complaint of left knee pain. The patient states the pain woke him from sleep and has been ongoing for several hours. He reports a past medical history of chronic left knee pain and psoriasis. His chronic knee pain has been waxing and waning for 6 months with moderate relief with ibuprofen, acetaminophen, and topical lidocaine. He has no prior surgeries, allergies, tobacco/alcohol/drug use, or recent sexual activity. He reports that he participated in high school football but did not sustain specific injuries to the knee. On review of systems, he reports no trauma, recent injury, fevers, chills, penile discharge, rash, or history of gout.
Initial vital signs were BP 140/72, HR 72, RR 16, T 36.7, and SpO2 99% and remained stable. Throughout the interview, he held his knee in a flexed position at approximately 30˚. On exam, he was noted to have a moderate to large left knee effusion. The left knee was warm compared to the right. He had generalized tenderness to palpation to the knee. The active range of motion was limited due to pain. The knee was able to be ranged passively from 0-110˚. No joint laxity was noted with anterior drawer, posterior drawer, varus, or valgus stress. His gait exam was antalgic and he avoided putting his full weight on his left knee.
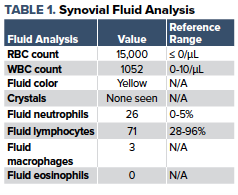
Given the patient's age, history, and exam, the differential was broad. It included psoriatic arthritis, juvenile idiopathic arthritis, gout, pseudogout, septic arthritis, osteomyelitis, fracture, meniscal injury, ligamentous injury, patellofemoral pain syndrome, osteochondral defect, and Osgood-Schlatter disease, among others. A CBC, BMP, ESR, CRP, urinalysis, and x-ray were ordered. An arthrocentesis was performed. The blood and urine studies were unremarkable. Synovial fluid analysis (Table 1) was not consistent with an infectious, or inflammatory etiology.
The x-rays (Figures 2 and 3) demonstrated a 9 mm free-floating osseous density without evidence of fracture and an irregularity of the lateral articular aspect of the medial femoral condyle, which was concerning for osteochondral defect. The patient reported significant pain relief after the aspiration of joint fluid. An ACE wrap was applied to the knee, he was provided with crutches, and made non-weight bearing until able to follow up in the orthopedic clinic.


Discussion
Osteochondral defect (OCD), historically referred to as Osteochondritis Dissecans, was described by Dr. Franz König more than 125 years ago. It is an acquired subchondral lesion characterized by osseous resorption, collapse, and sequestrum formation.4 OCD is a rare cause of joint pain with an incidence of 20 per 100,000 people.5 Patients aged 10-20 account for the majority of cases, although it may also be seen in adults. Incidence is 2-4 times higher in males than in females. The most common joint involved is the knee, with the lateral aspect of the medial femoral condyle being the most common location. Lesions can also be found in the ankle and elbow.4
There are many hypotheses regarding the etiology of OCD. They include inflammation, vascular deficiency, spontaneous osteonecrosis, genetics, and repetitive microtrauma. Currently, the most accepted of these is the microtrauma hypothesis. Many studies and case reports have suggested that repetitive trauma, frequently in the setting of athletic activity, may be the cause.2
Patients may present in one of three ways with pain during sports, pain with mechanical movement, or incidental findings in an asymptomatic individual. The most common symptom is pain with weight-bearing which is present in up to 80% of cases. A sudden increase in pain, or a joint effusion suggests an unstable lesion. The physical exam should be thorough as it can help rule out other potential etiologies.1
ED workup should begin with X-rays. Imaging of both knees should be obtained as 25% of cases have bilateral involvement.3 Serum and synovial fluid evaluation should be considered depending on the differential diagnosis. If imaging reveals concern for OCD, the knee should be immobilized, weight bearing and activity should be restricted, and the patient should be instructed to follow-up with orthopedics.
In the outpatient setting, MRI is used to help stage the lesion and determine operative vs non-operative management. Non-operative management strategies include immobilization, restricted weight-bearing, and activity restriction. Serial x-rays are obtained to assess for healing and the patient follows a gradual return to activity. Operative strategies include arthroscopy, chondral resurfacing, and osteochondral grafting.3,4 Most athletes return to sports with varied degrees of success.
Conclusion
Although OCD is a rare entity, emergency physicians should consider it in their differential for both traumatic and atraumatic joint pain. The diagnosis is made radiographically and is often missed by emergency medicine physicians and radiologists. These patients should be made non-weight bearing, restricted from all activity, and urgently referred to orthopedic surgery. A missed diagnosis can progress to chronic pain, mechanical symptoms, and early onset osteoarthritis.4
References
- Accadbled F, Vial J, Sales de Gauzy J. Osteochondritis dissecans of the knee. Orthopaedics & traumatology, surgery & research: OTSR. https://www.ncbi.nlm.nih.gov/pubmed/29197636. Published February 2018. Accessed February 18, 2020.
- Edmonds EW, Polousky J. A review of knowledge in osteochondritis dissecans: 123 years of minimal evolution from König to the ROCK study group. Clinical orthopaedics and related research. https://www.ncbi.nlm.nih.gov/pubmed/22362466. Published April 2013. Accessed February 18, 2020.
- Kocher MS, Tucker R, Ganley TJ, Flynn JM. Management of osteochondritis dissecans of the knee: current concepts review. The American journal of sports medicine. https://www.ncbi.nlm.nih.gov/pubmed/16794036. Published July 2006. Accessed February 18, 2020.
- Mohr B. Knee Osteochondritis Dissecans. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK538194/. Published February 17, 2019. Accessed February 18, 2020.
- Pallin DJ. Images in emergency medicine. Adolescent girl with knee pain. Annals of emergency medicine. https://www.ncbi.nlm.nih.gov/pubmed/19231671. Published March 2009. Accessed February 18, 2020.



