Radiology is a pillar of emergency care. What does the literature reveal about the impact of turnaround times in the radiology department?
Review of Literature
Radiology imaging delays as independent predictors of length of hospital stay for emergency medical admissions
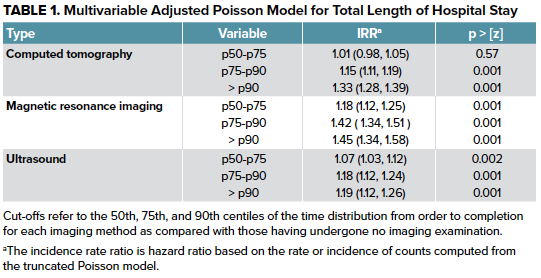
The authors studied the effects of computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound (US) TATs on hospital length-of-stay and cost of care for inpatients admitted from the ED. They found that a greater TAT was associated with longer hospital length of stay for all imaging modalities studied, and an increased cost of care was associated with greater usage of CT and MRI TATs.2 Although previous studies suggest that early advanced imaging may improve patient outcomes and decrease length-of-stays, these results illustrate that increased utilization of imaging may be a driver of increased length-of-stays and hospital costs. The authors suggest that a limited radiological imaging capacity may exacerbate imaging delays for inpatients from the ED. Therefore, as the inpatient demand for advanced imaging continues to increase, potential cost savings may be achieved through expanding radiological imaging capacity to decrease TAT, length-of-stay, and hospital costs.2
Practice policy and quality initiatives: decreasing variability in turnaround time for radiographic studies from the emergency department
The authors implemented quality improvement techniques at a large, full-service, tertiary-care hospital and studied their effects on ED radiograph TAT variability and ED throughput. The primary intervention was dissemination of daily TAT reports to radiologists to promote transparency and performance feedback (see Figure). Other interventions included changing radiology staffing and teaching radiologists’ practices to be more efficient. The results of the quality improvement initiatives are as follows:
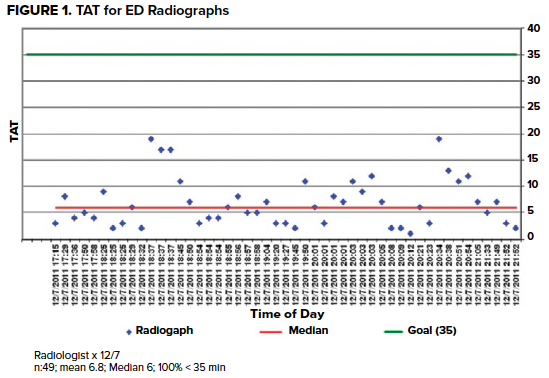
- The mean ED radiograph TAT decreased from 23.9 minutes to 14.6 minutes.
- The percentage of ED radiographs read within 35 minutes increased from 82.2% to 92.9%.
- The standard deviation of ED radiograph TAT decreased from 22.8 to 12.7.
- The mean ED “doctor to disposition” time for Emergency Severity Index class 4 or 5 patients decreased from 88.7 minutes to 79.8 minutes.
The authors suggest that the usage of standardized reports, workflow design improvements, and reading room enhancements can help optimize ED radiograph TAT variability and mean ED radiograph TAT. Since the mean ED “door to disposition” time decreased with improved TAT, efforts to decrease ED radiograph TAT may have the added benefit of improving patient flow.3
Improving Emergency Department radiology transportation time: a successful implementation of lean methodology
The authors implemented and evaluated the results of a Lean methodology-based intervention to decrease the plain radiograph transportation TAT, the time from when the study is ordered to the time when the study is completed, in the ED of a tertiary care center. The three primary Lean tools used by the authors are as follows:
- The authors assembled a kaizen team to engage stakeholders from various levels to achieve continuous process improvements.
- Value-stream mapping aided in identifying activities that added value as well as activities that did not, eliminating waste and redundancies.
- The authors employed kanban in the form of information systems that alerted radiologists to pull patients ready for imaging to the radiography suite.
The results of the intervention are as follows:
- The transportation TAT decreased from 22.9 minutes to 9.9 minutes.
- The percentage of patients being transported within 10 minutes increased from 32.3% to 71.6%.
- Patient length-of-stay decreased from 4.57 hours to 3.65 hours.
The authors conclude that Lean methodology and tools, such as those described above, can be employed with great success by ED administrators to improve TAT, throughput, and other key metrics in ED settings.4
SUMMARY OF LITERATURE
Prolonged radiology TAT contributes to a myriad of problems affecting ED operations including overcrowding, and negatively impacts metrics such as throughput, costs of care, and length-of-stays.1,2,5 Factors such as limited radiological imaging capacity have been shown to contribute to imaging delays.2 Recent studies illustrate that quality improvement initiatives that target human behavior, process design, and system issues have found considerable success in reducing mean TAT, TAT variability, and ED throughput.3,6 Lean methodology and tools have also been successfully applied to ED imaging transportation processes, resulting in decreased transportation TAT and length-of-stays.4,7-9 ED administrators can pursue similar interventions to improve process efficiency as well as key safety and quality metrics, leading to superior patient care and workflow.
LOOKING FORWARD/WHAT’S NEXT
Over the past two decades, technological breakthroughs such as picture archiving and communication systems (PACS) and speech recognition softwares have reduced radiology TATs from days to hours.3 Moreover, early advanced inpatient imaging, which is increasingly utilized, may improve outcomes but may be associated with longer TATs that can be addressed from an operational standpoint. In order to continue reducing the TAT and combat ED overcrowding and other challenges, more ED administrators are employing methodologies like Lean and Six Sigma to improve operational efficiency and deliver more exceptional patient care. Furthermore, certain Academic Emergency Medicine departments are beginning to consider quality improvement projects that seek to reduce CT burden in the ED by determining the extent to which certain urgent and emergent imaging studies alter disposition. More research is underway to investigate the best means to ascertain and address the impact of radiology TAT on ED operations.10,11
Other Recommended Literature
- van der Linden MCC, van Ufford HMEJ; Project Group Medical Specialists, van der Linden NN. The impact of a multimodal intervention on emergency department crowding and patient flow. Int J Emerg Med. 2019;12(1):21. Published 2019 Aug 27. doi:10.1186/s12245-019-0238-7
- England E, Collins J, White RD, Seagull FJ, Deledda J. Radiology report turnaround time: effect on resident education. Acad Radiol. 2015;22(5):662-667. doi:10.1016/j.acra.2014.12.023
- Rosenkrantz AB, Bonavita JA, Foran MP, Matza BW, McMenamy JM. Is there an association between radiologist turnaround time of emergency department abdominal CT studies and radiologic report quality?. Emerg Radiol. 2014;21(1):5-10. doi:10.1007/s10140-013-1164-2
- Bhayana R, Wang CD, Menezes RJ, Bartlett ES, Choi J. Optimising after-hours workflow of computed tomography orders in the emergency department. BMJ Open Qual. 2020;9(3):e000969. doi:10.1136/bmjoq-2020-000969
- Georgiou A, Prgomet M, Lymer S, Hordern A, Ridley L, Westbrook J. The Impact of a Health IT Changeover on Medical Imaging Department Work Processes and Turnaround Times: A mixed method study. Appl Clin Inform. 2015;6(3):443-453. Published 2015 Jul 8. doi:10.4338/ACI-2015-01-RA-0014
EMRA Administration & Operations Committee Links, Guides and Opportunities
- Check out what's happening with our group at the EMRA A&O landing page.
- Looking to gain a mastery of this and other relevant operational knowledge? Consider applying for EMRA's ED Directors Academy scholarship.
References
- Chong ST, Robinson JD, Davis MA, et al. Emergency Radiology: Current Challenges and Preparing for Continued Growth. J Am Coll Radiol. 2019;16(10):1447-1455. doi:10.1016/j.jacr.2019.03.009
- Cournane S, Conway R, Creagh D, Byrne DG, Sheehy N, Silke B. Radiology imaging delays as independent predictors of length of hospital stay for emergency medical admissions. Clin Radiol. 2016;71(9):912-918. doi:10.1016/j.crad.2016.03.023
- Towbin AJ, Iyer SB, Brown J, Varadarajan K, Perry LA, Larson DB. Practice policy and quality initiatives: decreasing variability in turnaround time for radiographic studies from the emergency department. Radiographics. 2013;33(2):361-371. doi:10.1148/rg.332125738
- Hitti EA, El-Eid GR, Tamim H, Saleh R, Saliba M, Naffaa L. Improving Emergency Department radiology transportation time: a successful implementation of lean methodology. BMC Health Serv Res. 2017;17(1):625. Published 2017 Sep 5. doi:10.1186/s12913-017-2488-5
- Succi MD, Yun BJ, Rao S, et al. Turning around cancer: Oncology imaging and implications for emergency department radiology workflow. Am J Emerg Med. 2020;38(2):317-320. doi:10.1016/j.ajem.2019.158435
- Perotte R, Lewin GO, Tambe U, et al. Improving Emergency Department Flow: Reducing Turnaround Time for Emergent CT Scans. AMIA Annu Symp Proc. 2018;2018:897-906. Published 2018 Dec 5.
- de Kok BM, Eijlers B, van der Linden MC, Quarles van Ufford HME. Lean-driven interventions, including a dedicated radiologist, improve diagnostic imaging turnaround time and radiology report time at the emergency department [published online ahead of print, 2020 Jun 24]. Emerg Radiol. 2020;10.1007/s10140-020-01803-3. doi:10.1007/s10140-020-01803-3
- Verbano C, Crema M. Applying lean management to reduce radiology turnaround times for emergency department. Int J Health Plann Manage. 2019;34(4):e1711-e1722. doi:10.1002/hpm.2884
- White BA, Yun BJ, Lev MH, Raja AS. Applying Systems Engineering Reduces Radiology Transport Cycle Times in the Emergency Department. West J Emerg Med. 2017;18(3):410-418. doi:10.5811/westjem.2016.12.32457
- Jalal S, Ante Z, Ouellette H, Peters S, Munk P, Nicolaou S. Impact of 24/7/365 Attending Radiologist Coverage on the Turnaround Time of Trauma-Related Imaging Studies Being Finalized Within 48 Hours in an Emergency Radiology Department, Offering a Perspective from a Tertiary Care Hospital [published online ahead of print, 2020 Mar 11]. Can Assoc Radiol J. 2020;846537120902046. doi:10.1177/0846537120902046
- Elzinga JL, Dunne CL, Vorobeichik A, et al. A Systematic Review Protocol to Determine the Most Effective Strategies to Reduce Computed Tomography Usage in the Emergency Department. Cureus. 2020;12(8):e9509. Published 2020 Aug 1. doi:10.7759/cureus.9509



