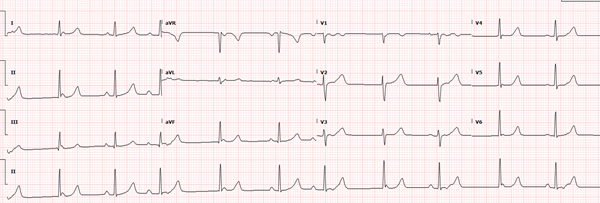
This ECG demonstrates a 2nd degree type I AV block (Mobitz I) with intermittent junctional beats, non-conducting P-waves, and retrograde P-waves.
Using the Lead II rhythm strip as a guide (see below), here’s the pattern:
- Junctional beat (narrow QRS with no preceding P-wave) followed immediately by a non-conducting sinus P-wave (↓)
- Sinus beat
- Sinus beat with longer PR (= Mobitz I) followed by a retrograde P-wave (↓) which resets the atrial conduction system (interrupting Mobitz I)
- Junctional beat (narrow QRS with no preceding P-wave) followed immediately by a non-conducting sinus P-wave (↓)
- Atrial conduction system resets and resumes pacing = sinus beat
- Sinus beat with longer PR (= Mobitz I) followed by a retrograde P-wave (↓) which resets the atrial conduction system (interrupting Mobitz I)
- Junctional beat (narrow QRS with no preceding P-wave) followed immediately by a non-conducting sinus P-wave (↓)
- Sinus beat followed by a retrograde P-wave(↓) which resets the atrial conduction system
- Junctional beat (narrow QRS with no preceding P-wave) followed immediately by a non-conducting sinus P-wave (↓)
- Sinus beat with retrograde P-wave (↓)
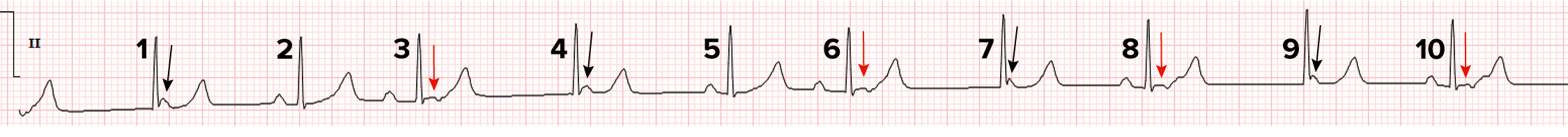
More on the retrograde P-waves (↓)
These P-waves are inverted in the inferior leads, which is expected for retrograde conduction. They reset the atrial conduction system, interrupting Mobitz I, so there isn’t the expected dropped QRS after a P-wave. Most likely, they conduct via the “retrograde only” accessory pathway since the AV node will be refractory to retrograde conduction that quickly following the QRS. Alternately, they conduct retrograde over a dual AV nodal pathway within the AV node. This is referred to as an echo beat or reciprocal beat, and typically follows a QRS preceded by a prolonged PR interval.
More on the non-conducting P-waves (↓)
After any beat with a retrograde P-wave, the atrial conduction system needs time to reset before it resumes pacing. During this time a junctional focus competes with the SA node. The junctional focus occurs just before the SA node impulse, so these P-waves are non-conducting because the rest of the conduction system has already depolarized from the junctional focus. These P-waves are sometimes entirely seen (after beat 4) and sometimes only partially seen (after beat 7) due to the close timing of the SA node in comparison to the junctional focus. These P-waves look like the other sinus P-waves, which is expected if they are all initiated in the SA node.
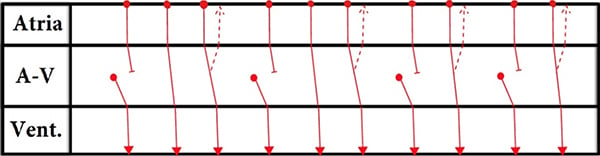
Ladder Diagrams
A ladder diagram uses lines with arrows and bars to illustrate the electrical activity within the cardiac conduction system that may not be evident on the surface EKG (ie, concealed conduction). It is constructed of 3 tiers that represent the atria, AV junction, and ventricle. The top horizontal line represents SA node, the 2nd horizontal line represents the beginning of AV conduction, and the 3rd horizontal line represents the end of AV conduction and the start of ventricular conduction. Solid circles represent the start of any impulse. Circles on the top line represent impulses originating from the SA node. Circles in the middle of the AV tier represent impulses originating in or around the AV node. Arrows indicate the direction of conduction and horizontal bars indicate a conduction block. Solid lines represent conduction via the fast pathway and dashed lines represent conduction via the slow pathway (or the accessory pathway in our case).
Read the description of the pattern (#1-10) while you work through this laddergram.
CASE COMMENTARY
By Ken Grauer, MD
This challenging case highlights the point that more than a single interpretation may be possible for a complex arrhythmia — and that sometimes, a definitive answer will only be forthcoming after EP study. We emphasize these principles:
- Awareness of the history may shed light on the probable mechanism of an arrhythmia. The patient in this case, a 19-year-old woman with a history of recurrent SVT episodes, was found on EP study to have an accessory pathway that was felt to participate in sustaining her arrhythmias.
- A laddergram clarifies our theory for the mechanism of this arrhythmia.
- Use calipers! This is the fastest way to enhance your ability to interpret complex arrhythmias — because it instantly allows you to assess intervals and regularity of the atrial and ventricular rate.
- When there are a number of elements in a given arrhythmia, it is helpful to assess the “easier-to-interpret” elements first.
- Try to determine if there is an underlying rhythm, such as sinus rhythm or atrial fibrillation. It is often much easier to figure out more complex elements after you have recognized the underlying rhythm.
- “Step back” to view the entire tracing before diving in to the details. Doing so may prove invaluable for recognizing certain phenomena such as “group beating.”
- Label sinus P-waves with arrows. This simple step will help you recognize which P-waves are probably conducting and which are not.
- Number the beats in order to intelligently discuss a complex rhythm with others.
- When an AV block is present in which some P-waves are conducted but others are not, a wonderful clue that a P-wave is probably conducting is if a beat occurs significantly earlier than expected.
Applying these principles to this tracing, begin by stepping back! You should notice the pattern of group beating: The appearance and interval duration for beats #1,2,3 and #4,5,6 are virtually identical. The same is true for beats #7,8 and #9,10. This is not by chance.
- The upright P-waves in the long lead II rhythm strip that are highlighted by red arrows are all sinus P-waves. The P-P interval shows no more than minimal variation except for the 3 relatively longer pauses (ie, between beats #3-4; 6-7; and 8-9). This indicates the underlying rhythm is sinus arrhythmia and that something else is probably accounting for these 3 much longer pauses. Looking for a cause of these pauses, we see the negative notch in the early part of the ST segment of beats #3, 6, 8, and 10 reveals the negative notch that indicates hidden atrial activity.
- There is no P-wave preceding beats #1, 4, 7, and 9. Since these QRS complexes look the same as all other QRS complexes, these 4 beats must be junctional escape beats. In support of this theory is the finding that the R-R intervals preceding beats #4, 7, and 9 are both equal and longer than the R-R interval preceding all other beats.
- Using calipers, it should now be easy to see that beats #2,3; 5,6; 8 and 10 are all preceded by an R-R interval that is shorter than the R-R interval preceding the junctional escape beats. This suggests all of these beats are probably conducted. The normal and equal PR intervals preceding beats #2, 5, 8, and 10 supports this theory. The fact that the PR interval preceding beats #3 and 6 is both equal and longer tells us there is progressive lengthening of the PR interval for conducted P waves within the first 2 groups — and that is the definition of Wenckebach!
Note: We cannot rule out the possibility that the negative deflections in the early part of the ST segment for beats #3, 6, 8, and 10 are PACs. Even if we knew these negative deflections represent retrograde atrial activity, we cannot say for certain from this single ECG that conduction is over the AP instead of a dual AV nodal pathway. That said, awareness of this patient’s history (ie, knowing she has recurrent SVT episodes with an AP) and knowing that retrograde conduction is facilitated by progressive preceding PR interval lengthening (which allows more time for retrograde conduction to occur) makes the mechanism illustrated in this laddergram the most plausible explanation. Retrograde conduction over an AP is a common substrate for facilitating orthodromic AVRT.
Dr. Grauer’s ECG Blog includes a primer on laddergrams.