Orbital cellulitis is an ophthalmologic emergency that requires immediate diagnosis and management; delayed diagnosis can pose a risk for vision loss and intracranial infectious extension. This case supports the use of bedside ultrasound in providing a timely and accurate diagnosis of orbital cellulitis.
Case Presentation
A 53-year-old-male presented to the ED for 7 days of right eye pain, blurry vision, and diplopia. The pain started while on a recent vacation. He denies any trauma, submersion injuries, or foreign body sensation. He had seen an ophthalmologist in an outside state and was prescribed a course of prednisone eye drops, which initially improved his symptoms. Several days later, the patient reported worsening of his symptoms with escalating pain, irritation, and swelling. Additionally, he progressed to developing diplopia and blurry vision, despite medication compliance. His symptoms were not associated with fevers, headaches, or changes in vision in the left eye.
Physical Exam
Physical exam was significant for right eye proptosis with restriction of primarily abduction and elevation. He experienced pain with movement in all directions and resistance to retropulsion. Evidence of mild lid edema and erythema without scleritis was also present. His visual acuity was 20/20 OS and 20/25 OD and his pupils were equal and reactive to light. Tonometer pressure in the right eye was 22 mmHg, compared to the left eye which was 12 mmHg. There were no rashes present on the face or body, mastoid tenderness, or inflammation of the tympanic membranes.
Lab/Imaging
Lab work revealed a white blood cell count of 6.4 [3.7-10.1 K/mm3], Lactic acid of 1.0 [0.7-2.0 mmol/L], ESR of 12 [0-15 mm/Hour], TSH of 0.91 [0.465-4.68 uIU/mL], Free T4 of 1.04 [0.78-2.19 ng/mL], and Total T3 of 1.60 [0.97-1.69 ng/mL].
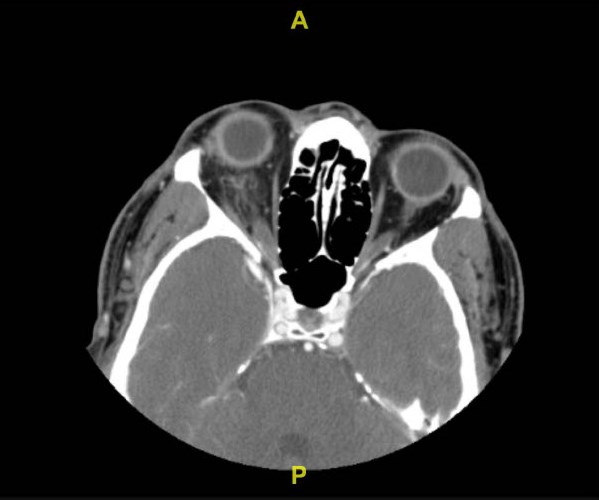
Bedside ultrasonography was performed by the emergency physician and was notable for fluid collection around the posterior globe itself without discernible abscess. CT scan of the orbit with IV contrast (Figure 1) demonstrated acute right orbital cellulitis with superimposed posterior scleritis, and optic perineuritis. Recommendations per ophthalmology were to start intravenous steroids along with broad-spectrum antibiotics. After antibiotics and steroids had been started, the patient was admitted to the hospital for continuation of medications as well as observation.

Figure 1. Initial CT of the orbit with IV contrast demonstrated acute right orbital cellulitis with likely superimposed posterior scleritis and optic perineuritis.
POCUS
Bedside ultrasonography was significant for free fluid posterior to the globe without discernible abscess. The linear probe was utilized on an ophthalmologic preset to obtain longitudinal and transverse images of the orbit. Longitudinal views of the right eye revealed a substantial volume of free fluid posterior to the globe with evidence of optic nerve enlargement and ill-defined margins (Figures 2 &3).
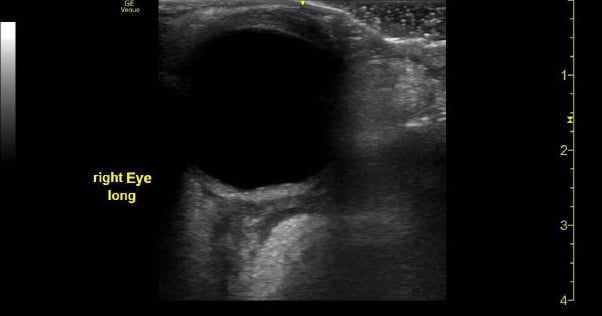
Figure 2. Hospital day 1 longitudinal view of the right eye using linear probe showed fluid surrounding the globe. Measurements of the optic nerve were 0.31 cm and 0.49 cm.
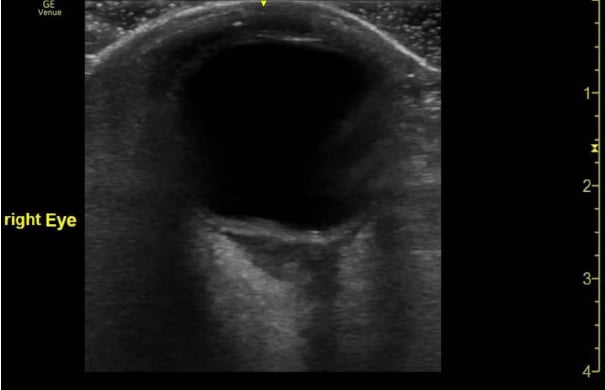
Figure 3. Hospital day 2 longitudinal view of the right eye using linear probe showed improvement of surrounding fluid around the globe.
Repeat bedside scans were performed during the patient’s stay in the hospital to monitor progression of disease and response to antibiotic therapy. Day 3 of admission showed a smaller volume of fluid consistent with radiographic improvement (Figure 4).
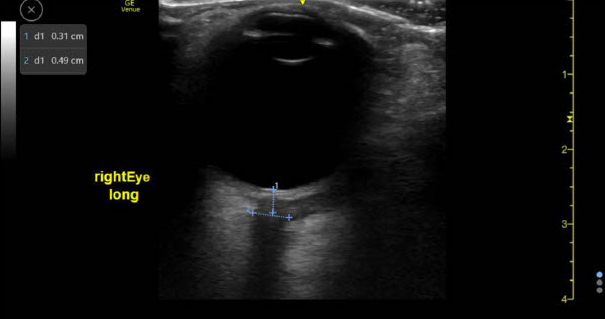
Figure 4. Right eye longitudinal view showed greater improvement of fluid collection compared to the previous day, although a small collection of fluid remained.
Discussion
Orbital cellulitis is an ophthalmologic emergency that requires immediate diagnosis and management; delayed diagnosis can pose a risk for vision loss and intracranial infectious extension. Point-of-care ultrasound proved to be useful in the initial diagnosis of orbital cellulitis and for assessing response to treatment.
Although ultrasound can be used for risk stratification of patients with non-specific eye complaints, it is unlikely to negate the need for advanced imaging such as CT and magnetic resonance imaging in patients with symptoms highly suggestive of orbital cellulitis (ie, ophthalmoplegia, proptosis, and impaired vision).2 However, ultrasound may prove to be the preferred imaging modality in pediatric and uncooperative patients who may not tolerate a contrast-enhanced CT scan in the ED setting.
This case supports the use of bedside ultrasound in providing a timely and accurate diagnosis of orbital cellulitis.
Case Conclusion
The patient received IV methylprednisolone 125 mg for acute inflammation, as well as vancomycin 3,072 mg, piperacillin/tazobactam 4.5 g, and ceftriaxone 2 g for broad-spectrum antibiotic coverage.
Ultrasound re-evaluation on hospital day 2 showed improvement of periorbital swelling and the posterior orbital fluid. By hospital day 3, there was almost complete resolution of symptoms as well as a significant decrease in the fluid surrounding the globe. Physical exam showed improvement of ocular movement in all directions, with reduced pain and proptosis.
Following antibiotic completion in the hospital, the patient was continued on amoxicillin/clavulanic acid for an additional 7 days and prednisone 80 mg for 28 days with a taper.
Disclaimer: This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
References
- Maw AM, Huebschmann AG, Mould-Millman NK, Dempsey AF, Soni NJ. Point-of-care ultrasound and modernization of the bedside assessment. J Grad Med Educ. 2020;12(6):661–665.
- Basraoui D, Elhajjami A, Jalal H. Imaging of orbital cellulitis in children: about 56 cases. Pan Afr Med J. 2018;30:94.
- Tsirouki T, Dastiridou AI, Ibánez Flores N, Cerpa JC, Moschos MM, Brazitikos P, Androudi S. Orbital cellulitis. Surv Ophthalmol. 2018;63(4):534-553.