Editor's Note: The print version of this article inadvertently omitted authors Charles Kennedy and Meera Gebrael. Please note (and forgive) the error.
Case
A 26-year-old female presented to the ED complaining of 2 weeks of progressively worsening shortness of breath and left sided chest pain. The patient had been seen at a private clinic the week prior due to cough, congestion, chest pain, and intermittent shortness of breath. A chest x-ray was done at that time which showed an enlarged heart and she was subsequently instructed to follow-up with her primary care physician (PCP) for a cardiology referral. She was seen in her PCP’s office one week later where an EKG was performed which revealed no acute abnormalities and an outpatient transthoracic echocardiogram (TTE) was ordered. The next day she presented to the ED due to worsening chest pain and subjective fevers. She stated that her chest pain was worse when lying flat and alleviated when she leaned forward however her physical exam was unremarkable and all vital signs were within normal limits. She then had a bedside TTE performed by the emergency physician which revealed a large pericardial effusion and an 8cm mass adjacent to the right atrium (Figures 1-2). On exam, she clinically had no signs of cardiac tamponade and was well-appearing.
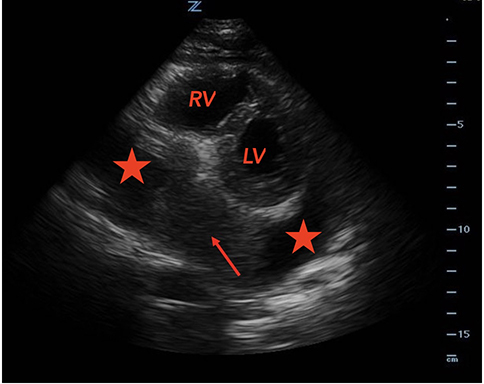
Figure 1. Parasternal transthoracic echocardiography in the short axis (PSAX). The arrow indicates a large mass adjacent to the right atrium. The two stars indicate the large pericardial effusion. LV = Left Ventricle. RV= Right Ventricle
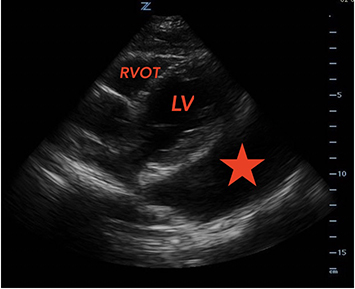
Figure 2. Parasternal transthoracic echocardiography in the long axis (PSAX). The star indicates a large pericardial effusion. LV = Left Ventricle. RVOT = Right Ventricle Outflow Tract
A subsequent CT of the chest showed a large low-density pericardial effusion with a large heterogeneously enhancing mass likely arising from pericardium (Figure 3-4). The mass was located at the base of the heart abutting the inferior vena cava (IVC) and right atrium and was favored to represent a pericardial angiosarcoma. The patient was admitted to the cardiology service where a pericardiocentesis and biopsy were performed and 1100cc of bloody fluid was removed. The pericardial fluid was primarily composed of red blood cells and mixed inflammatory cells suggestive of a hemorrhagic effusion. Ultimately, the patient had an uneventful hospital course and was discharged from the hospital with a plan for her to follow up to discuss her biopsy results. A few days later the cytology on the pericardial fluid came back positive for synovial sarcoma. She was awaiting follow-up with both Cardiothoracic Surgery and Hematology/Oncology.

Figure 3. Coronal CT scan of chest. The straight red line is showing the size of the mass. The star indicates the large pericardial effusion.

Figure 4. Sagittal CT scan of chest. The straight red line is showing the size of the mass. The star indicates the large pericardial effusion. LV = Left ventricle
Background
Primary cardiac neoplasms are extremely rare with an incidence of 0.0001%. Primary cardiac synovial sarcomas (PCSS) account for < 5% of cardiac sarcomas and < 0.1% of all primary cardiac tumors.3 Prognosis is extremely poor in cases of PCSS with a median survival rate of < 9 months.4 PCSS is a rapidly progressive tumor which can present with non-specific symptoms such as chest pain, shortness of breath, weight loss, and fatigue. Patients usually remain asymptomatic until the tumor increases to a certain size or until spread and metastases occur. Additionally, pericardial effusions and subsequent cardiac tamponade are possible complications. Advanced tumors may spread to the opposite side of the heart by the time they are discovered. Symptoms usually present when mass effect of the tumor or obstruction of blood flow from the pulmonary veins occurs.1 Diagnosis of PCSS is often achieved later in the disease course due to the generalized symptoms associated with it and the rarity of the disease. However, with increasing use of TTE in clinical and emergency department settings, a more rapid diagnosis can be made. Furthermore, transesophageal echocardiography (TEE), which has a sensitivity of 97% for detecting cardiac masses, is also becoming more common in specialty clinics and inpatient settings. TEE can be used to gain more information about the tumor’s characteristics such as shape, size, and precise location.5 In this article we describe a case in which the diagnosis and treatment of PCSS was expedited by the use of point-of-care TTE.
Discussion
Primary cardiac neoplasms are extremely rare, with an incidence of 0.0001%.3 Because of the nonspecific clinical signs and symptoms associated with the disease, diagnosis can be challenging; often, preliminary detection first occurs through imaging techniques such as X-Ray or CT scan.
According to a review of the literature of PCSS, patients presenting with cardiac synovial sarcomas have a mean age of 32.5 years with a range of 13 to 66 years old. It is more common in males than in females, with a ratio of 3.5:1, and it has previously demonstrated a predisposition for young adults and adolescents. Also, the right side of the heart is more commonly affected, with a ratio of 2:1.
PCSS can also be associated with significant pericardial effusions and signs of congestive heart failure. Obstruction of blood flow within the heart and infiltration of the myocardium is often the cause of death in these patients. Because of the high fatality rate of these malignancies, rapid detection and early resection of PCSS, before invasion of the heart or metastasis can occur, offer the best chance of extending life expectancy. However, due to the rapid infiltration and aggression of the malignancy it is often detected when it has already advanced into the myocardium, complicating complete resection. When compared to left sided PCSS, right sided PCSS appear more infiltrative and are more likely to metastasize. This suggests that neoadjuvant chemotherapy may be of some benefit to help shrink the tumor before complete resection. Cases of right-sided PCSS that were treated with neoadjuvant chemotherapy along with surgical resection reported a median survival time of 27 months.8 Unfortunately, complete resection is often not achievable because of tumor inaccessibility and the risk of affecting other cardiac structures. However, even in cases of partial tumor resection, surgical intervention has proven to increase prognostic survival time and has shown some benefit in regard to tumor control.8,9 Patients who underwent surgical intervention showed a median survival time of 14 months compared to 9-12 months for medical therapy alone.8,9
Because of the rapidly progressive course of PCSS and the risk of metastases in primarily right-sided cardiac tumors, early detection is paramount in accelerating diagnosis and initiating the treatment process. Previous literature has shown that echocardiography is the primary method of evaluating the tumors, with a 97% sensitivity. Specifically, a TTE can assess location, shape, size, degree of adherence, and mobility of the tumor,6 whereas TEE provides information about the specific insertion point of the tumor. In addition to echocardiography, CT should be used to gain a better understanding of the complexity of the mass and to check for metastasis.6 In the case described here, TTE has been shown to be a relatively quick and effective way to evaluate for a cardiac mass with an associated pericardial effusion.
Conclusion
Diagnosing a primary cardiac synovial sarcoma can prove challenging because of the nonspecific nature of the symptoms and rarity of the disease. Furthermore, the risk of complications associated with the disease and the high mortality rate make early detection and intervention essential. By utilizing bedside echocardiography in the ED, we can expedite workup, help guide treatment options, and most importantly, identify life-threatening emergencies that would benefit from immediate intervention.
References
- Varma T, Adegboyega P. Primary cardiac synovial sarcoma. Arch Pathol Lab Med. 2012;136(4):454-458.
- Leja MJ, Shah DJ, Reardon MJ. Primary cardiac tumors. Tex Heart Inst J. 2011;38(3):261-262.
- Miller DV, Deb A, Edwards WD, Zehr KJ, Oliveira AM. Primary synovial sarcoma of the mitral valve. Cardiovasc Pathol. 2005;14(6):331-333.
- Talukder M, Joyce L, Marks R, Kaplan K. Primary cardiac synovial sarcoma. Interact Cardiovasc Thorac Surg. 2010;11(4):490-492.
- Riles E, Gupta S, Wang DD, Tobin K. Primary cardiac angiosarcoma: A diagnostic challenge in a young man with recurrent pericardial effusions. Exp Clin Cardiol. 2012;17:39-42.
- Butany J, Yu W. Cardiac angiosarcoma: two cases and a review of the literature. Can J Cardiol. 2000;16(2):197-205.
- Varma T, Adegboyega P. Primary cardiac synovial sarcoma. Arch Pathol Lab Med. 2012;136(4):454-458.
- Blackmon SH, Reardon MJ. Surgical treatment of primary cardiac sarcomas. Tex Heart Inst J. 2009;36(5):451-452.
- Antonuzzo L, Rotella V, Mazzoni F, et al. Primary cardiac angiosarcoma: a fatal disease. Case Rep Med. 2009:591512.


