Here it is: the dreaded pediatric elbow. Is it a fracture? An ossification center? Shouldn't there be a bone there? No, it's Superman.
Radiographic assessment of acute pediatric elbow trauma requires a firm grasp of developmental anatomy, radiographic landmarks, and common injury patterns. By using a systematic approach to reading elbow x-rays delineated below, you can begin to feel more confident and adept at evaluating the subtle signs of pediatric fractures.
Why is the pediatric elbow difficult?
The challenge comes from the complex developmental anatomy with multiple ossification centers that mature at different ages. The multiple ossification centers may be difficult to differentiate from fractures in the acute traumatic setting. Familiarity with age-variable anatomy is crucial for an accurate diagnosis.
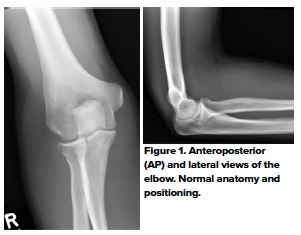
1. Ensure adequate films
An AP film should be obtained with the elbow in full extension and the forearm supinated (Fig 1). For the true lateral projection, the elbow should be flexed 90 degrees with the forearm supinated. The routine use of comparative views is not recommended, as it comes at a considerable cost of radiation exposure to the child;1 several studies have shown that the routine use of comparative views does not alter patient management.2,3
2. Look for joint effusion and soft tissue swelling
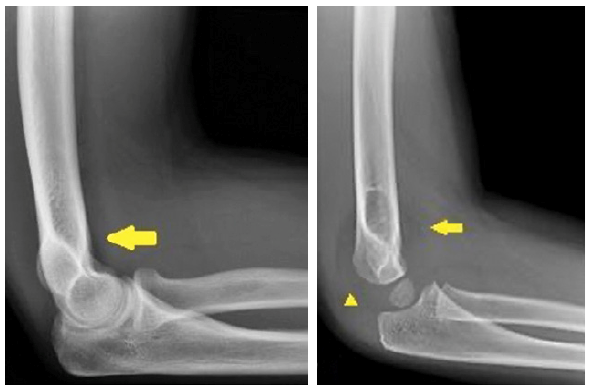
The elbow fat pads are situated external to the joint capsule. On a true lateral radiograph, the normal anterior fat pad is seen as a radiolucent line parallel to the anterior humeral cortex; and the posterior fat pad is invisible.
Distention of a structurally intact joint causes displacement of the fat pads - the posterior fat pad moves posteriorly and superiorly and becomes visible; the anterior fat pad becomes more sail-like.4 (Fig 2)
On the lateral x-ray of the elbow, a joint effusion can be inferred when there is displacement of the anterior fat-pad or presence of the posterior fat pad. An elbow joint effusion without a visible fracture seen on radiographs can suggest an occult fracture and should prompt further evaluation.

A study by Major et al.5 showed that a joint effusion without visible fracture seen on conventional radiographs is often associated with an occult fracture and bone marrow edema on MRI. The study found that 57% of imaging where the only finding was joint effusion had a fracture and 100% had bone marrow edema on MRI. In cases where an occult fracture is suspected, follow-up radiographs in 7-10 days can be obtained to evaluate for the presence or absence of sclerosis or periosteal new bone formation as indicators of healing. For suspected occult fractures, standard of care remains posterior elbow splinting with follow-up radiographs at 7-10 days.
3. Check bone alignment
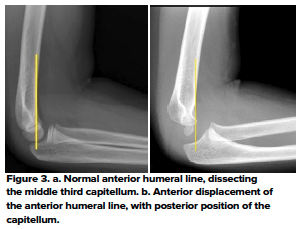
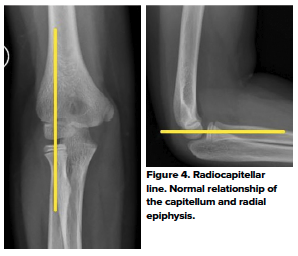
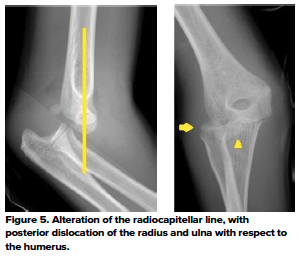
The anterior humeral and radiocapitellar lines are used to assess elbow alignment. The lines assess the geometric relationship of one bone to the other. Malalignment usually indicates fractures.
The anterior humeral line is drawn along the anterior cortex of the humerus and should bisect the middle third of the capitellum. Malalignment indicates a fracture - in most cases, posterior displacement of the capitellum in a supracondylar fracture. This sign relies on adequate ossification of the capitellum and therefore is reliable in children over the age of 4 years only.6 (Fig 3)
The radiocapitellar line evaluates the relationship of the proximal radius to the capitellum on all views (Fig 4). If the integrity of this line is compromised, then dislocation should be suspected (Fig 5)
4. Identify ossification centers
There are 6 secondary ossification centers in the elbow. They ossify in a sex- and age-dependent predictable order. CRITOE is a mnemonic for the sequence of ossification center appearance. (Table 1 and Fig 6)
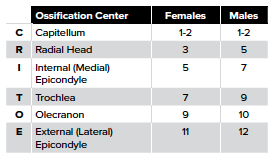
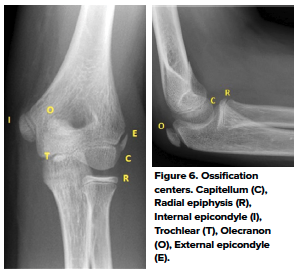
The medial epicondyle fuses to the shaft of the humerus at 13 years for females and 15 years for males. The growth plates are vulnerable to traction or shearing forces which result in fracture and/or apophyseal injuries. Displaced epicondyle fractures can be missed if the normal pattern of ossification development is not recognized.7
5. Identify Distal Humeral Fractures
Distal humeral fractures in pediatric patients include supracondylar, lateral condylar, medial epicondylar, medial condylar, and lateral epicondylar fractures. It is vital to correctly identify the fracture, as management varies greatly depending on the fracture (and severity). Following is a review of these fractures.
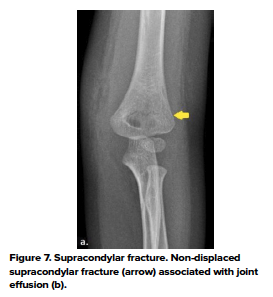
- Supracondylar fractures
- The most common pediatric elbow fracture is the supracondylar fracture, accounting for 50%-70% of cases, with a peak age of 6-7 years old.8 At this age, significant bony remodeling of the supracondylar process occurs, causing cortical thinning and predisposing to fracture. Falls onto an outstretched hand account for 95% of supracondylar fractures, causing hyperextension stress on the elbow.8 The severity of a supracondylar fracture is identified using the Gartland classification, which is helpful in delineating management. Important complications of supracondylar fractures include neuropraxia (including anterior interosseous nerve, radial nerve, and ulnar nerve palsies) and vascular compromise. (Fig 7)
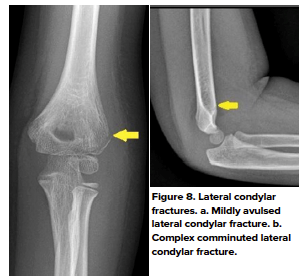
- Lateral condylar fractures
- Lateral condylar fractures are the second most common pediatric elbow fracture, accounting for 10%-15% of elbow fracture, with a peak age of 6-10 years old.9 Patients usually present with lateral elbow pain after a FOOSH with the forearm in supination, creating a varus force on the elbow. A nondisplaced lateral condylar fracture is often very subtle and challenging to detect on conventional radiographs. Joint effusion and soft tissue swelling may provide secondary signs as to the presence of the lateral condylar fracture. (Fig 8 a,b)
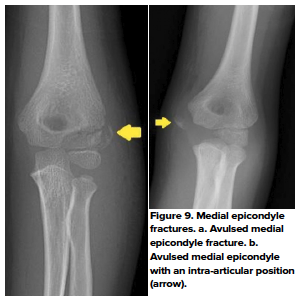
- Medial epicondylar fractures
- Fractures of the medial epicondyle make up approximately 12% of all pediatric elbow fractures.10 These fractures are typically due to valgus stress at the elbow joint such as from a posterior dislocation, a fall, or throwing, and usually occurs as an avulsion fracture.10 Peak injury is between 7-15 years old. Usually, patients will present with their elbow in flexion with associated pain at the medial aspect of the joint. Throwing mechanisms of injury may be described by patients as a “popping” sensation just prior to onset of pain. (Fig 9 a,b)
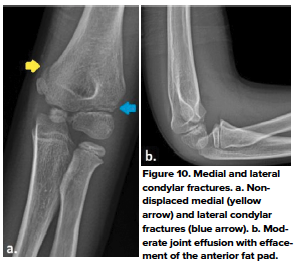
- Medial condylar fractures
- Medial condylar fractures are uncommon, accounting for less that 1% of all distal humeral fractures in children. These fractures usually occur in children 8-14 years of age after a fall onto an outstretched hand. Typically these fractures present with medial soft tissue swelling with pain in the condylar region. It is difficult to distinguish between these and medial epicondylar fractures, however, these usually are NOT related to dislocation.10 (Fig 10 a, b)
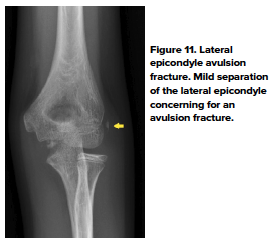
- Lateral epicondylar fracture
- Lateral epicondylar fractures are extremely rare and usually occur between ages 9-15 years. In the older child, these fractures are due to a direct blow to the lateral epicondylar region and are usually associated with other injuries of the elbow.11 In younger children, avulsion forces from the forearm extensor muscles are responsible, likely due to a reaction mechanism.7 Pain and soft tissue swelling of the lateral epicondylar region are common complaints from patients with this fracture (Fig 11).
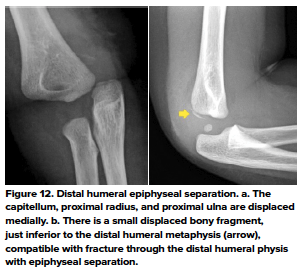
- Distal Humeral Epiphyseal Separation
- This fracture is rare and has been described in children less than 2 years of age. Common mechanisms include FOOSH, traction, and rotary forces. A considerable force is required to cause this fracture, and since young infants are not mobile enough to produce this force, non-accidental trauma must be suspected in these cases. That being said, it can also occur due to birth trauma- both vaginal delivery and cesarean section. The diagnosis can be challenging since the distal humeral epiphysis is cartilaginous and not visualized on x-rays. The most important finding is the posteromedial displacement of the radius and ulna in relation to the distal humerus.12 (Fig. 12)
Identify Radial and Ulnar Fractures
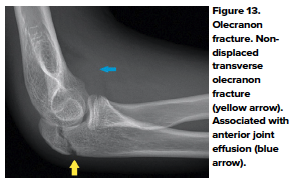
- Olecranon Fracture
- Olecranon fractures occur in children from a direct blow to the elbow or from a FOOSH. Clinical presentation includes pain and swelling with point tenderness over the olecranon. Most fractures are greenstick fractures, however, special attention should be made in regards to whether the fracture is extra-articular vs intra-articular. Always look for an associated injury, especially dislocation/fracture of the radial head.14 (Figure 13)
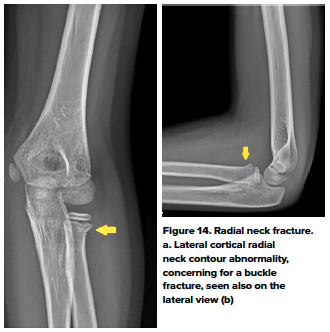
- Proximal Radial Fracture
- Proximal radial fractures can occur in the radial head or the radial neck. Most common mechanisms of injury include FOOSH with the elbow extended or posterior dislocation of the elbow. Patients present with tenderness over the radial head with pain localized to the lateral aspect of the elbow with pronation and supination. Radial neck fractures typically are classified as Salter Harris II fractures through the physis, and radial head fractures are intra-articular and typically occur in older children or adolescents.13 (Fig 14)
7. Management
If a fracture is suspected, immediate orthopedic consultation is recommended. In cases of closed displaced fractures, a prompt reduction may be necessary. A fracture should be splinted in a position of function until outpatient orthopedic follow-up is available. After placement of the splint, check that the extremity is neurovascularly intact.
Upon discharge, include ED return precautions, information on splint care, and provide a sling. Cases that require immediate attention in an operating room include open reductions, inability to reduce with procedural sedation, and any contraindications to procedural sedation.
References
- Johnson KL, Bache E. In Pediatric skeletal trauma - Techniques and applications. Berlin Heidelberg New York: Springer; 2008.
- Chacon D, Kissoon N, Brown T, Galpin R. Use of comparison radiographs in the diagnosis of traumatic injuries of the elbow. Ann Emerg Med. 1992;21 (8):895-899.
- Kissoon N, Galpin R, Gayle M, Chacon D, Brown T. Evaluation of the role of comparison radiographs in the diagnosis of traumatic elbow injuries. J Pediatr Orthop. 1995;15(4):449-453.
- Goswami GK. The fat pad sign. Radiology. 2002;222:419-420.
- Major NM, Crawford ST. Elbow effusions in trauma in adults and children: is there an occult fracture?. AJR Am J Roentgenol. 2002;178(2):413-418.
- Herman MJ, Boardman MJ, Hoover JR, Chafetz RS. Relationship of the anterior humeral line to the capitellar ossific nucleus: Variability with age. J Bone Joint Surg Am. 2009;91(9):2188-2193.
- Wilkins KE. Fractures and dislocations of the elbow region. In: Rockwood CA, Wilkins KE, King RE, eds. Fractures in Children, 3rd ed. Philadelphia: JB Lippincott, 1991. pp. 526-617
- Alburger PD, Weidner PL, Betz RR. Supracondylar fractures of the humerus in children. J Pediatr Orthop. 1992;12:16-19.
- Jacoby SM, Herman MJ, Morrison WB, et al. Pediatric elbow trauma: An orthopaedic perspective on the importance of radiographic interpretation. Semin Musculoskelet Radiol. 2007;11:48-56.
- Patel NM, Ganley TJ. Medial Epicondyle Fractures of the Humerus: How to Evaluate and When to Operate. J Pediatr Orth. 2012;32:S10-S13.
- Kilborn T, Moodley H, Mears S. Elbow your way into reporting paediatric elbow fractures - A simple approach. SA J Radiol. 2015;19(2).
- Supakul N, Hicks RA, Caltoum CB, Karmazyn B. Distal humeral epiphyseal separation in young children: an often-missed fracture-radiographic signs and ultrasound confirmatory diagnosis. AJR Am J Roentgenol. 2015;204(2):W192-W198.
- Lins RE, Simovitch RW, Waters PM. Pediatric Elbow Trauma. Orthop Clin North Am. 1999; 30(1):119.