Case
A 97-year-old-female presents to the ED with left hip pain after a mechanical fall at home. Her left lower extremity is shortened and externally rotated, and she yells in pain when it is manipulated. Radiographs confirm what you already suspected: a left hip fracture. You try to keep her comfortable while she waits for a hospital bed, but she continues to groan in pain despite multiple doses of IV morphine. Not wanting to continue with opioids, you consider alternative options.
Background
Hip fractures are common injuries evaluated in the ED. The majority of patients who suffer a hip fracture are over 80 years old, and as the population ages, the incidence of hip fractures is expected to increase.1 These injuries can be extremely painful and debilitating. Pain management is crucial not only for patient comfort but also because sufficient analgesia decreases complications and promotes postoperative mobility.1 Although emergency physicians are unlikely to be involved in postoperative care, they are typically the first clinician to evaluate these patients and thus frequently responsible for minimizing patient discomfort in the initial stages.
Opioids have long been a mainstay for treatment of pain; however they are associated with side effects including constipation, sedation, respiratory depression, and dependence.2 Regional anesthesia can be a useful and appropriate alternative. Techniques such as the femoral nerve block, 3-in-1 femoral nerve block, and fascia iliaca block are relatively safe, fairly effective, and avoid the use of opioids.3 However, these blocks may not be providing adequate analgesia based on the innervation of the hip.3,4
Since the anterior hip capsule receives most of the sensory input of the hip,4 any nerve block should ideally target the nerves that supply this area. A recent anatomic study has confirmed that the anterior hip capsule is innervated by the obturator nerve, accessory obturator nerve, and the femoral nerve.5 Because of the way that the high articular branches of the femoral nerve and accessory obturator nerves course, there is some concern that consistent blockade of these nerves is not achieved with the fascia iliaca block and the 3-in-1 femoral nerve block.3,6 Furthermore, it has also been suggested that these techniques do not reliably block the obturator nerve.6,7 The anterior inferior iliac spine (AIIS) and iliopubic eminence (IPE) have been identified as key landmarks where articular branches of the nerves course.5 Based on this information, the pericapsular nerve group (PENG) block was developed in 2018 to specifically target these articular branches.3 The creators of this technique reported achieving pain reduction while avoiding motor blockade after performing this block on five patients with varying hip pathology including intertrochanteric fractures, subcapital fractures, and metastases of the femoral head and acetabulum.3
Below, we describe how to perform this novel technique.
Performing the PENG Block
To perform this block, we advocate a two-person approach where one individual is responsible for using ultrasound (US) to guide and maintain the block needle in place while the other person injects the anesthetic.
Setup
Two syringes should be attached to a three-way stopcock. One syringe should contain local anesthetic and the other should contain normal saline. One end of IV tubing should be connected to the stopcock and the other end to a spinal needle. This device will facilitate administration of anesthetic (Figure 1).

Positioning
The patient should be supine with the operator standing on the ipsilateral side of the affected extremity. The US machine should be placed so that the screen is in a direct line of sight.
Landmark Identification
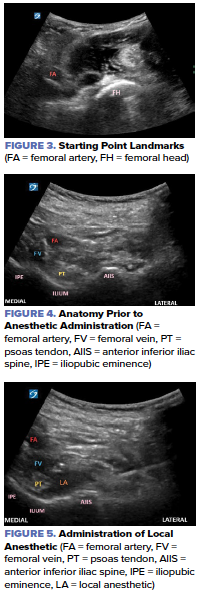
A low-frequency curvilinear probe should be placed in a transverse orientation at the proximal thigh and over the femoral head. The probe should then be rotated 45 degrees so that it is parallel to the inguinal crease.
Visualize and identify the femoral head and femoral artery (Figure 3). While maintaining the femoral artery in view, slide the probe cephalad until the ilium, the AIIS and the IPE come into view with the psoas tendon located just on top of the ilium (Figure 4). The target for anesthetic placement is the osseous surface of the ilium just below the psoas tendon.

Performing the Procedure
As nerve blocks are typically done with aseptic technique, the skin should be prepped in a sterile fashion, and a sterile cover should be placed on the probe. Apply sterile gel to the skin and again identify the landmarks for the block. While maintaining the probe in a firm position, identify the needle insertion site for in-plane approach. The insertion site is approximately 2 cm away from the probe.
Using a 27g needle, inject a small amount of local anesthetic to create a skin wheal at the intended needle insertion site. Then, begin inserting a 20-22g block needle in line with the probe and adjust as needed until the needle can be visualized on the US screen. If satisfied with the projected path of the needle, continue to advance the needle until it reaches the desired location just deep to the psoas tendon. After ensuring that the needle has penetrated the overlying fascia layer, aspirate to confirm that vasculature was not accidentally punctured. Begin hydrodissection with small amounts of sterile normal saline to lift the psoas tendon from the ilium. Visualizing the elevation of the psoas tendon confirms that the needle is in the correct position, and the operator can begin injecting local anesthetic (Figure 5).
The volume of the anesthetic will be determined by a weight-based approach to avoid toxicity. In general, the total volume for this block will be near 40-50 cc. Typically, the anesthetic volume will need to be supplemented with sterile normal saline. It is important to note that if the operator is experiencing pressure while injecting, the needle should be readjusted into the space below the psoas tendon to avoid injection into muscle or tendon.
How Effective is the PENG Block?
In theory, the PENG block has certain advantages in comparison to other existing hip blocks. Because it encompasses a larger selection of sensory nerves, the PENG block should result in more extensive analgesia which may potentially result in less opioid use.6 Furthermore, as the PENG block targets the sensory nerves, it may avoid motor blockade which would allow for earlier mobilization by patients.6
Because the PENG block is relatively new, most of the available literature on its effectiveness consists of case reports and case series. A comprehensive literature review identified 74 patients who received the PENG block, the vast majority of whom were undergoing surgery or arthroplasty.6 Overall, utilization of the PENG block, whether in isolation or in combination with other blocks, resulted in decreased pain and administration of opioids.6 No serious adverse events were reported, and only two patients experienced quadriceps weakness, likely due to deposition of anesthetic in unintended locations.6 Although promising, it is difficult to evaluate the efficacy of this block given the lack of observational studies and randomized-controlled trials.6
There are several trials in progress comparing the PENG block to other blocks. One double-blinded study comparing the PENG block to the femoral nerve block demonstrated that patients who received the PENG block reported significantly less pain in the recovery room and maintained better quadriceps strength than those receiving the femoral nerve block.1
Although this block appears to be most commonly performed by anesthesiologists in the perioperative setting, successful utilization of this block in the ED has been described. Luftig et al report that use of the PENG block in the ED provided three patients with pelvic fractures enough analgesia such that they were able to move the hip with minimal or no discomfort.8
Though more studies are needed to validate its performance and ability to spare motor function, the PENG block has already shown great potential for alleviating acute hip pain in the ED.
REFERENCES
- Lin D-Y, Morrison C, Brown B, et al. Pericapsular nerve group (PENG) block provides improved short-term analgesia compared with the femoral nerve block in hip fracture surgery: a single-center double-blinded randomized comparative trial. Reg Anesth Pain Med. 2021;46(5):398-403.
- Benyamin R, Trescot AM, Datta S, et al. Opioid complications and side effects. Pain Physician. 2008;11(2 Suppl):S105-20.
- Girón-Arango L, Peng PWH, Chin KJ, Brull R, Perlas A. Pericapsular nerve group (PENG) block for hip fracture. Reg Anesth Pain Med. 2018;43(8):859-863.
- Acharya U, Lamsal R. Pericapsular nerve group block: an excellent option for analgesia for positional pain in hip fractures. Case Rep Anesthesiol. 2020;2020:1830136.
- Short AJ, Barnett JJG, Gofeld M, et al. Anatomic Study of Innervation of the Anterior Hip Capsule: Implication for Image-Guided Intervention. Reg Anesth Pain Med. 2018;43(2):186-192.
- Morrison C, Brown B, Lin D-Y, Jaarsma R, Kroon H. Analgesia and anesthesia using the pericapsular nerve group block in hip surgery and hip fracture: a scoping review. Reg Anesth Pain Med. 2021;46(2):169-175.
- Swenson JD, Davis JJ, Stream JO, Crim JR, Burks RT, Greis PE. Local anesthetic injection deep to the fascia iliaca at the level of the inguinal ligament: the pattern of distribution and effects on the obturator nerve. J Clin Anesth. 2015;27(8):652-657.
- Luftig J, Dreyfuss A, Mantuani D, Howell K, White A, Nagdev A. A new frontier in pelvic fracture pain control in the ED: Successful use of the pericapsular nerve group (PENG) block. Am J Emerg Med. 2020;38(12):2761.e5-2761.e9.



