A 10-year-old otherwise healthy female presented to the ED with bilateral posterior mandibular facial swelling that had begun earlier that day without trauma.
The onset of her symptoms occurred while she was playing video games approximately 2 hours prior to arrival. She did not report any symptoms other than mild bilateral facial pain and a feeling of fullness in her cheeks. Her parents noted that the swelling occurred without any identifiable precipitating factor.
Initial physical examination demonstrated mild swelling around the mandibular angles with no erythema or induration present. Intraoral examination revealed no signs of dental trauma, mucosal swelling, drainage, or posterior erythema. Crepitus was felt throughout the patient’s anterior neck extending to the mastoids, indicating subcutaneous air.
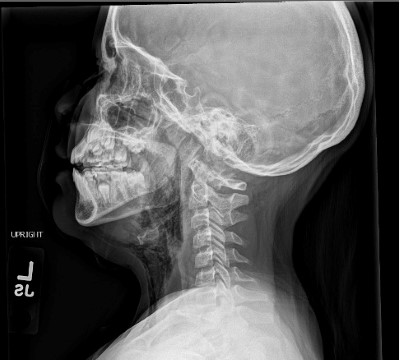
Soft tissue radiographs demonstrated subcutaneous air extending from the anterior neck and lower face bilaterally. Otolaryngology was consulted, and a diagnosis of pneumoparotid was made. The patient was discharged with ENT follow-up and antibiotics.
Discussion
Pneumoparotid/pneumoparotitis is an uncommon cause of parotid gland swelling classified by free air seen within the parotid glands. Typically, swelling of the parotid glands can be attributed to infection, autoimmune disease, obstruction, or benign growths.
In this case, the cause of retrograde flow of air into the parotid gland was likely an insufficient Stensen’s Duct. This is the duct that typically allows for anterograde flow of serous saliva from the parotid gland into the oral cavity.2 There is no identified cause of an insufficient duct, although average measurements of Stensen’s Ducts are 5 cm long and 1.7 mm in diameter.1 Shorter, wider ducts would be at a higher risk of insufficiency, allowing retrograde flow into the gland itself.
Since 1987, only 54 cases of pneumoparotid have been reported in literature. The majority of these cases (74%) are in the pediatric population and are linked to psychological stresses or tic disorders. All cases can be linked to an increase in intraoral pressure, whether self-induced or iatrogenic/idiopathic.2 It was reported that childhood stresses could range from conflicts with parents to an excuse to not attend school. It was also reported iatrogenically in patients receiving CPAP.2 Although seen as bilateral in this case, unilateral cases have been reported.
Stensen’s Duct is formed sometime during the 6th-12th week of development to transport the parotid secretions.8 The parotid glands consist of clusters of acinar cells, which create the serous saliva; interspersed are fatty adipocytes and duct cells.3 When air enters the parotid gland, it insufflates completely to the level of the acinar cells. Acinar cells are low-pressure systems connected by tight junctions with minimal myoepithelial cell support.3 A consequence of insufflating these cells is rupturing these acinar complexes, causing air to track along the cervical fascial planes.
Crepitus felt on exam should lead clinicians to obtain further imaging. As the name implies, simple pneumoparotid will show air within the parotid glands, while pneumoparotitis will have observable inflammatory changes and pain.2 These changes can be as subtle as mild erythema at the opening of Stensen’s Duct, or as obvious as purulent discharge with mandibular erythema.4
Radiographic evidence can be obtained through multiple modalities, depending on the institution’s capabilities. In this case, plain film X-ray was utilized given the patient’s age and parent knowledge and comfort, showing subcutaneous emphysema tracking along the patient’s anterior neck and to the angles of both mandibles.
Computed tomography (CT) is the gold standard and gives excellent visualization of the extent of intraglandular air as well as extraglandular air in subcutaneous tissue.5 CT with thinner slices is preferable to identify any complicating pathology such as stones or abscesses. Ultrasound may be utilized and can help demonstrate air within the gland.6This can be seen as a ring-down effect while using a linear probe.

Management of pneumoparotitis/pneumoparotid is focused on infection prophylaxis and ensuring resolution of subcutaneous air. Otolaryngology (ENT) consultation and follow-up is recommended to ensure resolution. Infection of simple pneumoparotid is a feared complication that can lead to abscess formation or spread of infection through fascial planes. Penicillin is recommended as a prophylactic antibiotic treatment.
Case Conclusion
The patient was discharged with ENT follow-up and antibiotics. During two subsequent follow-up appointments, resolution of subcutaneous air occurred, no infection was reported, and a possible cause was brought to light. The patient reported blowing up a pool toy with minimal pain the day before and blowing into a closed fist just prior to her symptoms beginning.
Overall, pneumoparotid is a condition that is generally self-induced and self-limited. Physical exam and imaging is pertinent to accurate diagnosis, and ENT consultation is recommended to ensure complete resolution.
References
- Togni L, Mascitti M, Santarelli A, et al. Unusual conditions impairing saliva secretion: Developmental anomalies of salivary glands. Frontiers in physiology. Published July 3, 2019. Accessed June 17, 2022.
- Gazia F, Freni F, Galletti C, et al. Pneumoparotid and pneumoparotitis: A literary review. International Journal of Environmental Research and Public Health. 2020;17(11): 3936.
- Igbokwe CO. Ultrastructure of the Parotid Salivary Gland in the Greater Cane Rats (Thryonomys Swinderianus). J Microsc Ultrastruct. 2018 Jan-Mar;6(1):17-22. Retrieved June 17, 2022.
- McGreevy AE, O'Kane AM, McCaul D, Basha SI. Pneumoparotitis: A case report. Head & Neck. 2012;35(2).
- Madhavan AA, Carr CM, Carlson ML, Lane JI. Imaging Findings Related to the Valsalva Maneuver in Head and Neck Radiology. American Journal of Neuroradiology. 2019.
- Ghanem M, Brown J, McGurk M. Pneumoparotitis: a diagnostic challenge. Int J Oral Maxillofac Surg. 2012 Jun;41(6):774-6.
- Mather AJ, Stoykewych AA, Curran JB. Cervicofacial and mediastinal emphysema complicating a dental procedure. J Can Dent Assoc. 2006 Jul-Aug;72(6):565-8.
- Chason HM, Downs BW. Anatomy, Head and Neck, Parotid Gland. Updated 2021 Oct 5. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.



