Takotsubo cardiomyopathy (TTC), also known as stress-induced cardiomyopathy or "broken heart syndrome," is a transient cardiac dysfunction often triggered by physical or emotional stress.3 Although the exact pathophysiology remains unclear, excessive catecholamine release and autonomic dysregulation are considered primary mechanisms. This case report describes a 34-year-old female who developed TTC following an intentional overdose of risperidone, fluoxetine, oxcarbazepine (Trileptal), loratadine, and cyproheptadine, highlighting the potential role of these medications in the development of severe cardiac dysfunction.
Case Presentation
A 34-year-old female with a history of major depressive disorder and anxiety disorder was brought to the emergency department after being found wandering around by police. The patient disclosed to police that she had taken 10 of her Prazosin pills. The patient was sent to the Emergency Department where they proceeded to call poison control. Poison control recommended medical clearance after an observation for 6 hours in the Emergency Department. During her emergency department stay, the patient was acting appropriately and EKG showed sinus tachycardia with normal intervals. She was noted to have dilated pupils and mild urinary retention. Between hour 6 and 7 of her Emergency Department stay, the patient became increasingly agitated and was thus admitted for further observation. Shortly after being admitted, the patient became increasingly somnolent and was eventually noted by her Emergency Room tech to be unresponsive. The patient was then intubated and sedated and sent to the ICU. Upon arrival to the ICU, collateral information was obtained and patient’s sister noted empty bottles of recently filled prescriptions of:
- fluoxetine 10 mg, quantity 21
- cyproheptadine 4 mg, quantity 7
- Trileptal 150 mg, quantity 42
- Risperdal 1 mg, quantity 14
- Loratadine 10 mg, quantity 7
Poison control was updated on the patient’s status and recommended charcoal.
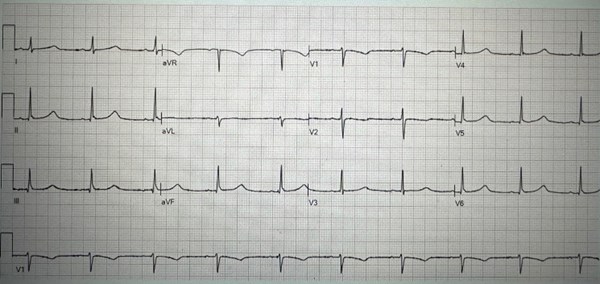
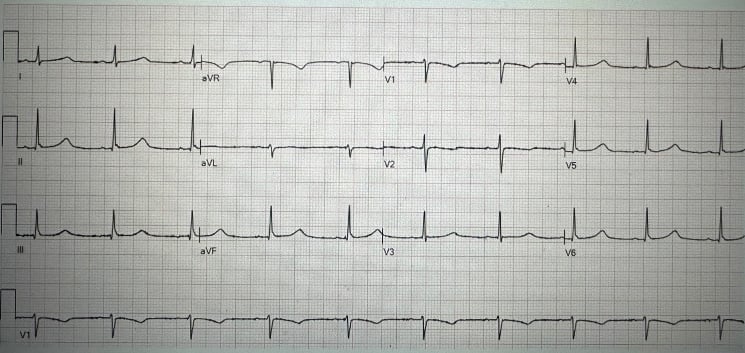
Repeat electrocardiogram (ECG) revealed a prolonged QT interval of 552 ms with T-wave inversions in V1 and V2.
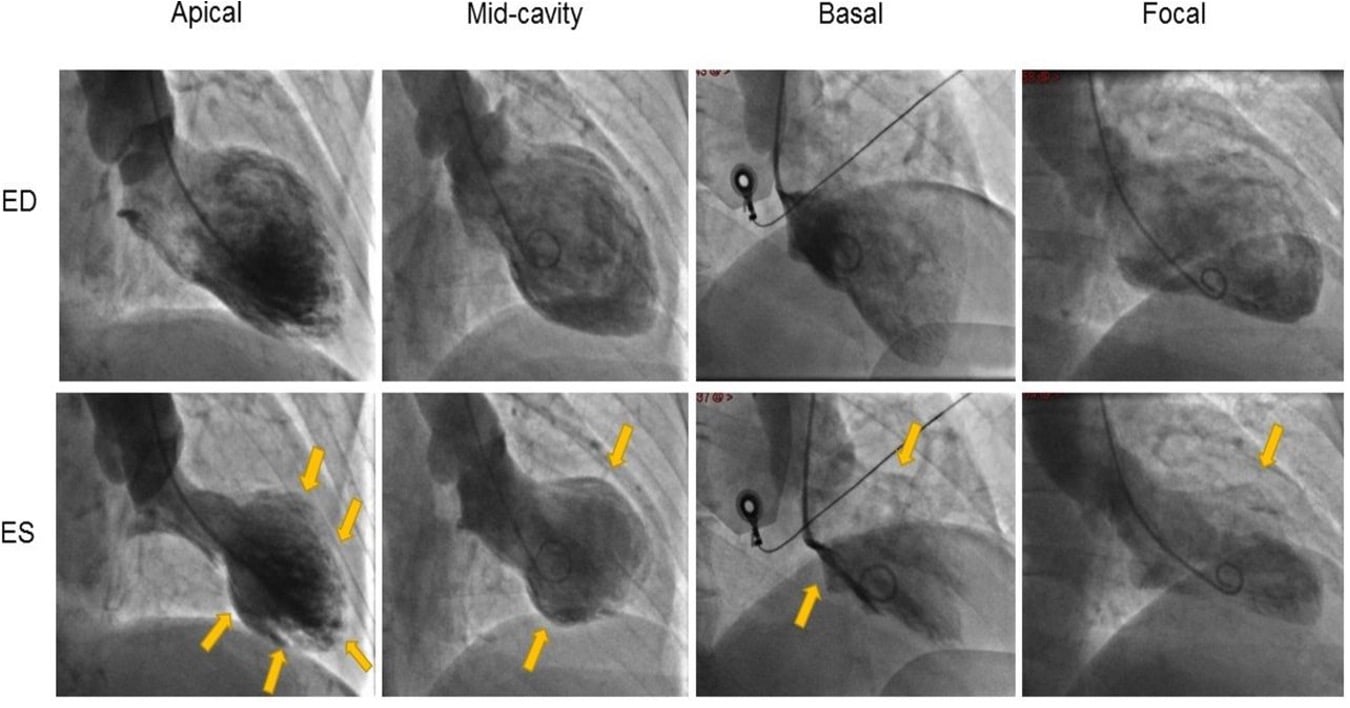
Three days into hospitalization, an echocardiogram was performed due to persistent hemodynamic instability, revealing an ejection fraction (EF) of 10-15% with akinesis of the entire apical myocardium and a hyperdynamic basal segment, findings consistent with Takotsubo cardiomyopathy. Coronary angiography was negative for obstructive coronary disease.
Discussion
This case underscores the potential cardiovascular toxicity associated with psychiatric and antihistamine medications, particularly in overdose situations. Risperidone is known to prolong the QT interval, predisposing patients to arrhythmias.1,4 Fluoxetine, an SSRI, has been linked to autonomic dysregulation and increased sympathetic activity.6 Oxcarbazepine can contribute to electrolyte disturbances, while cyproheptadine, an antihistamine with anticholinergic properties, may also influence autonomic tone. Antipsychotic-induced heart failure is a consequence of prior direct cardiac lesions in response to drug stimuli. These pathological lesions included myocarditis, cardiomyopathy, ischemic heart diseases, etc.2,5
The combined pharmacologic effects likely contributed to a catecholamine surge and subsequent myocardial dysfunction characteristic of TTC.
The patient was managed with supportive care, including beta-blockers and ACE inhibitors. Over the course of two weeks, her ejection fraction improved to 55-60%, and she was successfully extubated and converted to tracheostomy with gradual neurological recovery. Her psychiatric medications were re-evaluated, and adjustments were made to minimize future cardiovascular risks.
Conclusion
This case highlights the potential for Takotsubo cardiomyopathy following an intentional overdose involving medications known to influence autonomic and cardiovascular function. Clinicians should be aware of the risks of QT prolongation, autonomic instability, and catecholamine surges associated with psychiatric and antihistamine medications. Prompt recognition and supportive management can lead to favorable outcomes.
References
- Cubeddu LX. Drug-induced Inhibition and Trafficking Disruption of Ion Channels: Pathogenesis of QT Abnormalities and Drug-induced Fatal Arrhythmias. Curr Cardiol Rev 2016; 12: 141-154.
- Coulter DM, Bate A, Meyboom RH, Lindquist M, Edwards IR. Antipsychotic drugs and heart muscle disorder in international pharmacovigilance: Data mining study. BMJ 2001; 322: 1207-1209.
- Dawson DK. Acute stress-induced (Takotsubo) cardiomyopathy. Heart 2018;104:96-102.
- Haddad PM, Anderson IM. Antipsychotic-related QTc prolongation, torsade de pointes and sudden death. Drugs 2002; 62: 1649-1671.
- Kilian JG, Kerr K, Lawrence C, Celermajer DS. Myocarditis and cardiomyopathy associated with clozapine. Lancet 1999; 354: 1841-1845.
- Polcwiartek C, Kragholm K, Schjerning O, Graff C, Nielsen J. Cardiovascular safety of antipsychotics: a clinical overview. Expert Opin Drug Saf 2016; 15: 679-688.