A thyroid storm is an acute, life-threatening emergency that requires timely recognition and management. Left untreated, the mortality rate is 80-100%.
A 37-year-old female presents to a community ED intensely concerned about left shoulder pain of 2 months duration. She complains of weakness, fatigue, palpitations, dyspnea on exertion, and lower extremity edema occurring inconsistently for the past 6 months. She appears restless with pressured speech, but otherwise looks her stated age.
On physical examination she is tachycardic with a heart rate of 161, febrile to 101.8F, and tachypneic with 26 respirations per minute. Her blood pressure is mildly elevated at 152/93, and she is saturating at 100 percent on room air. Generally, she appears agitated and thin. She is very anxious and is concerned that she cannot stay in the hospital much longer because of her PTSD. A large, firm thyroid large firm thyroid is noted. She is tachycardic with a regular rhythm, and her abdomen is soft. On the patient's lower extremities you note mild pretibial edema.
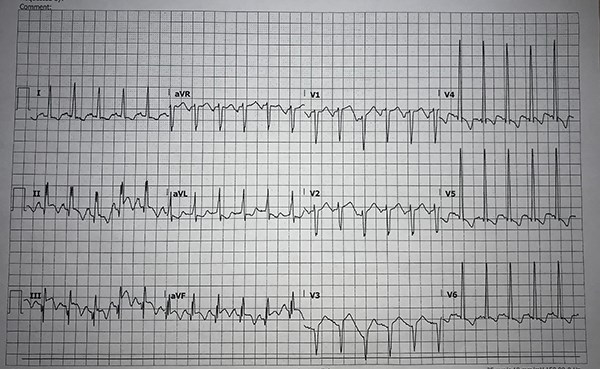
This presentation is odd, but anxiety, tachycardia, age, and enlarged thyroid gland mean thyroid storm is on the differential diagnosis. Basic elements in the evaluation of this patient include: EKG, TSH, free T4, CBC, CMP, and glucose. The results of these tests demonstrate a low TSH, elevated T4, and EKG demonstrating ST elevation in leads II, III, and aVF with reciprocal lateral lead depression. Elevated thyroid hormone levels, decreased TSH, fever, agitation, and acute cardiac pathology further support concern for thyroid storm.
What Is Thyroid Storm?
A thyroid storm is an acute, life threatening emergency characterized by a hypermetabolic state precipitated by the presence of excessive thyroid hormone. If untreated, mortality rates in patients with a thyroid storm are between 80% and 100%, and with timely management mortality is still estimated between 15% and 50%.1
The basic pathophysiology operating as the driving force behind a thyroid storm is a hyperadrenergic state occurring as a result of primary hyperthyroidism leading to increased T3 and T4 release from the thyroid, or secondary hyperthyroidism directed by excessive TRH leading to elevated levels of TSH.
A plethora of underlying diseases can degenerate into a thyroid storm, but Graves' disease is by far the most common, accounting for approximately 85% of cases in the U.S.1 Often, this presentation arises in an individual with baseline hyperthyroidism exacerbated by infection, MI, pregnancy, trauma, or other stressors.
Recognition and Initial Management
Recognizing an acute thyroid storm is critically important. Severe presenting symptoms include:
- Hyperpyrexia
- Tachycardia
- CHF
- Dysrhythmia
- Agitation
- Anxiety
- Delirium
- Liver dysfunction
- Psychosis
Diagnosis of thyroid storm hinges on the presence of the aforementioned severe, life-threatening symptoms paired with laboratory evidence of hyperthyroidism. Elderly patients must be diagnosed with caution, as they can present with an apathetic thyroid storm where fever and hyperactivity are absent.1
The Burch-Wartofsky Point Scale is a useful tool for identifying a thyroid storm. Patients score points for dysfunction in thermoregulation, the gastrointestinal system, or the hepatic system as well as tachycardia, atrial fibrillation, evidence of heart failure, and changes in neurologic status. Patients presenting with thyroid storm and associated neuropsychiatric symptoms should be managed carefully because they are at an increased risk for mortality.2
Management of a thyroid storm focuses on 5 critical components in a stepwise approach:
- Supportive care
- Beta-blockade
- Inhibiting the new synthesis of thyroid hormone
- Preventing the release of new thyroid hormone
- Stopping peripheral conversion
Supportive care is key; control fever with antipyretics and cooling. Benzodiazepines can be considered for anxiolysis, along with crystalloid fluids for rehydration.
Next, administer beta-blockers to mitigate the peripheral effects of elevated thyroid hormone. This is commonly accomplished with propranolol, which also alleviates agitation and tremor; be sure the patient does not have underlying heart failure or pulmonary disease.
Thalidomides such as propylthiouracil and methimazole inhibit new synthesis of thyroid hormone. Meanwhile iodine can be administered to block the release of pre-stored hormone.
Finally, hydrocortisone or dexamethasone can prevent peripheral conversion of thyroid hormone.
Case Management
Following these 5 steps, careful thought should be given to the underlying cause of the clinical presentation. Additionally, in patients with thyroid storm, neuropsychiatric symptoms portend a high risk presentation. In this case the patient's psychiatric symptoms are concerning.
If a desire to leave against medical advice is expressed, this should be approached cautiously. The question of whether the patient has decision-making capacity should be raised early following diagnosis of thyroid storm, and their ability to understand the risks of signing out from the hospital against medical advice should be carefully considered.
References
1. Idrose AM. Acute and Emergency Care for Thyrotoxicosis and Thyroid Storm. Acute Med Surg. 2015;2(3): 147–157.
2. Swee du S, Chng CL, Lim A. Clinical characteristics and outcome of thyroid storm: a case series and review of neuropsychiatric derangements in thyrotoxicosis. Endocr Pract. 2015;21(2):182-189.