Part 2 of a 3-part series: Pulmonary artery catheters (PACs) are considered a valuable diagnostic and management tool in cardiogenic shock. (Read Part 1 here.)
What is a Swan-Ganz (PA) Catheter?
Swan-Ganz or Pulmonary Artery Catheters (PACs) were developed by Drs. Jeremy Swan and William Ganz in the 1960s-1970s as a means of invasive hemodynamic monitoring in critically ill patients.1 Often placed at the bedside with relative ease, PACs are inserted through a central line into the right heart and advanced into the pulmonary artery. They are capable of providing valuable information about cardiac output, right-sided heart pressures, and oxygenation.2
Indications
Pulmonary artery catheters are primarily used for hemodynamic monitoring in the setting of cardiogenic shock, assisting in determining the etiology of undifferentiated shock, and evaluation of fluid status. They are often helpful in guiding the management of patients with heart failure. PACs can also be used in the evaluation of pulmonary hypertension or pericardial diseases such as constrictive pericarditis and cardiac tamponade. These devices are frequently used in cardiothoracic surgery for preoperative planning and in the intraoperative and postoperative phases for close hemodynamic monitoring.3
Contraindications
Absolute contraindications to PAC insertion include right ventricular assist device (RVAD) device presence and central line insertion through an active infection site. Right-sided endocarditis and right-sided heart tumors/masses are also largely considered to be absolute contraindications.4 History of pulmonary artery rupture is an additional absolute contraindication due to a high risk of recurrence, as well as small pulmonary vessels. Relative contraindications to PAC insertions include significant coagulopathy. Preexisting left bundle branch block is another relative contraindication due to the risk of development of a right bundle branch block which could lead to complete heart block.3
Parts of the Device
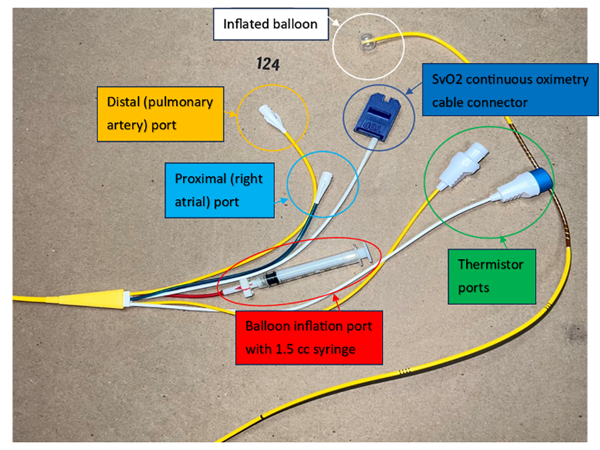
PA catheters are 110 cm long and typically range from 5 to 8 French in diameter. They contain a distal port (typically yellow, as shown in Figure 1 below) that corresponds to the catheter tip, a proximal port (typically blue) that connects to the a lumen terminating 30 cm from the tip, and a balloon inflation port. Some catheters have additional accessory ports for measurement of mixed venous oxygen saturation (SvO2) and cardiac output (CO) via thermodilution.
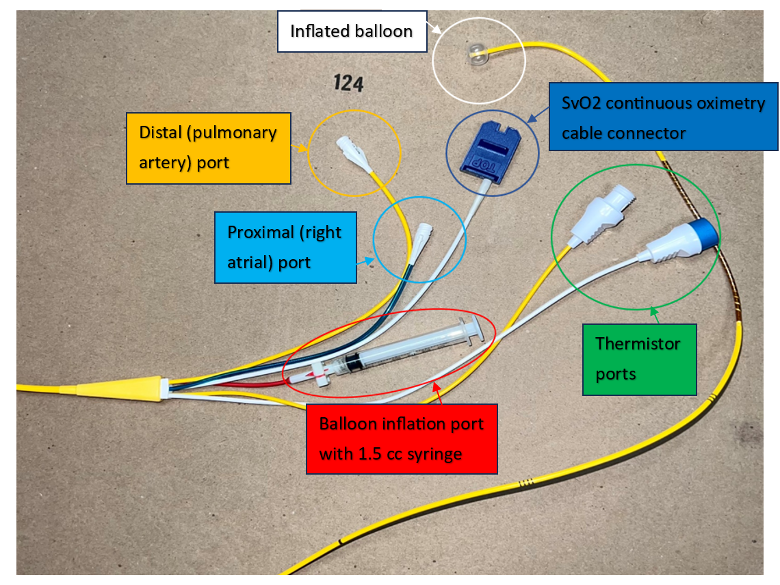
Figure 1. PA catheter parts. Abbreviations: SvO2, mixed venous oxygen saturation.
Device Insertion
As with any procedure, obtain consent and perform a time-out prior to beginning. Select the insertion site prior to procedure set-up, ideally using ultrasound visualization. Potential sites include the internal jugular, subclavian, femoral, or less commonly the antecubital veins, with the right internal jugular vein typically being the site of choice. The right internal jugular and left subclavian veins typically allow for the most anatomically efficient passage into the heart.5 A longer catheter and fluoroscopy may be required for more distal insertion sites (femoral, antecubital). The PAC can also be floated over a wire inserted into an existing central venous catheter (CVC) site.
Gather the following equipment:
- PA catheter
- Introducer with protective sheath
- Sterile saline flushes
- Lidocaine, 10-cc syringe, and 25-gauge needle
- 18-gauge introducer needle
- Scalpel
- Guidewire
- Needle driver, sutures, and scissors
- Adhesive dressing
- Ultrasound machine, sterile probe cover, and gel if placing under ultrasound guidance
- Code cart with defibrillator and transcutaneous pacer
- Telemetry equipment
- Fluoroscopic equipment if needed
Prime the PA catheter:
- Cap and flush the introducer sheath and PAC ports with sterile saline
- Place the sterile sheath over the catheter
- Test balloon by inflating with 1.5 milliliters (mL) air, evaluating for leaks (perform only after placing the sterile sheath over the catheter, otherwise there is potential to tear the balloon as it passes through the sheath)
- Place the sterile sheath over the catheter
- Connect transducer and pressure tubing to the catheter
Position and prepare the patient: Place the patient in either Trendelenburg position if using the jugular or subclavian vein, or supine position if selecting a femoral or antecubital vein. Wash your hands and don a sterile gown, cap, and gloves. Prep the skin with appropriate cleaning solution such as chlorhexidine and establish a sterile field using a sterile drape. Apply the sterile probe cover to the ultrasound probe. After again manually palpating or visualizing the target vessel with ultrasound, inject a local anesthetic agent (typically 1-2% lidocaine) using the 25-gauge needle to numb the expected tract. An additional IV anxiolytic or analgesic may be considered as needed.
Place the introducer using Seldinger Technique: Insert the 18-gauge introducer needle into the target vein through the anesthetized tract. Apply negative pressure on the syringe while advancing, and stop when blood is aspirated. Ideally confirm the location of the needle tip in the vein and not adjacent artery using ultrasound, and then remove the syringe. Confirm the return nonpulsatile dark red blood flow before inserting the guidewire through the needle.5 Remove the needle. Using ultrasound, confirm that the wire is located within the vein and remains in the vein when scanning distally. Subsequently use the scalpel to create a skin nick alongside the wire, and place the introducer sheath and obturator over the guidewire, advancing it into the vein. Remove the guidewire and obturator from the sheath. Attach a sterile flush to the port and aspirate blood to ensure adequate flow. Secure the introducer to the skin with sutures and a sterile dressing.
Float the PA catheter: Attach the distal port of the PAC (typically yellow) to the pressure monitor, setting the pressure to zero once the catheter tip is level with the patient's heart. Advance the PAC through the introducer up to 15 cm. At this point the PAC tip will have emerged from the introducer sheath, and the balloon can be inflated. After inflating the balloon, continue to advance the PAC while observing the pressure waveforms on the monitor. Ensure that the balloon is fully inflated each time the catheter is advanced and fully deflated each time it is withdrawn.
Each cardiac chamber/vessel has a distinctive waveform, which can be used to identify the location of the catheter tip (Figure 2). Slowly advance the catheter through the right atrium, followed by the right ventricle, followed by the pulmonary artery. Advancing beyond this will produce a pulmonary artery wedge pressure waveform as illustrated in Figure 2 below. This is the most distal location for catheter insertion. Once pressure waveforms have been obtained in all of the specified locations, deflate the balloon and re-confirm presence of the associated pulmonary artery pressure waveform (Figure 2).
Normal PAC Waveforms
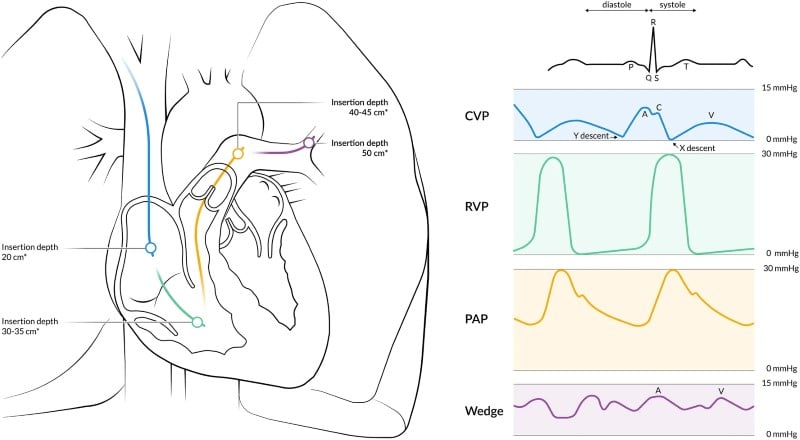
Figure 2. Normal waveforms. Abbreviations: CVP, central venous pressure; RVP, right ventricular pressure; PAP, pulmonary artery pressure. (Image from Bootsma et al., 2022; open-access article)6
Right Atrial Pressure/Central Venous Pressure
In the right atrium, the PAC measures the central venous pressure.7 This tells us venous return as well as right ventricular end-diastolic pressure. There are three positive deflections and two negative deflections in a normal RA waveform (Figure 2). Normal right atrial measurements are between 0 to 10 mmHg.6
Positive deflections (a, c, v) occur when the pressure in the right atrium increases. The a wave represents atrial contraction, the c wave occurs during tricuspid valve closure, and the v wave occurs due to passive atrial filling while the ventricle is contracting.6
Negative deflections (x, y) occur when the right atrial pressure is decreasing. The x wave represents atrial relaxation and the y wave represents atrial emptying/early ventricular filling.6
Right Ventricular (RV) Pressure Waveform
The RV waveform measures the peak right ventricular systolic pressure and the right ventricular end-diastolic pressure.7 It is characterized by a steep, rapid upslope during ventricular systole (Figure 1). Normal RV systolic pressures are between 15 to 28 mmHg. The diastolic pressure in a healthy individual is 0 mmHg.6
Pulmonary Artery Pressure (PAP) Waveform
The pulmonary artery waveform measures both the systolic and diastolic pressure within the PA.7 A normal PAP waveform has 4 phases. The first is a rapid, steep systolic upstroke followed by a systolic downslope. The next phase is the diastolic notch which occurs when the pulmonary valve closes. Lastly, the pressure decreases back down (Figure 2). The normal PAP pressure is between 14 and 28 mmHg. The normal diastolic PAP pressure is between 6 and 16 mmHg. The normal mean PAP pressure is between 10 and 22 mmHg.6
You can distinguish between the RV waveform and the PAP waveform by the slope of the pressure during diastole. The PAP will have a downward slope during diastole whereas the RV will have an upward slope during diastole. Note that the peak systolic pressure in the RV and PAP should be similar.
Pulmonary Artery Wedge Pressure
The pulmonary artery wedge pressure measures the left atrial pressure and can estimate left ventricular end-diastolic pressure.7 The wedge pressure is measured when the balloon on the catheter is inflated and stops all distal flow of blood. The PAWP reflects the left atrial pressure. It has two positive deflections (a and v wave) and two negative deflections (x and y wave).6 A normal PAWP is between 5 and 12 mmHg.
Similar to the right atrial waveform, the a wave represents atrial systole and the v wave represents passive atrial filling and right ventricular systole. The x wave descent represents atrial diastole and the y descent represents atrial emptying (Figure 2).
Abnormal Waveforms
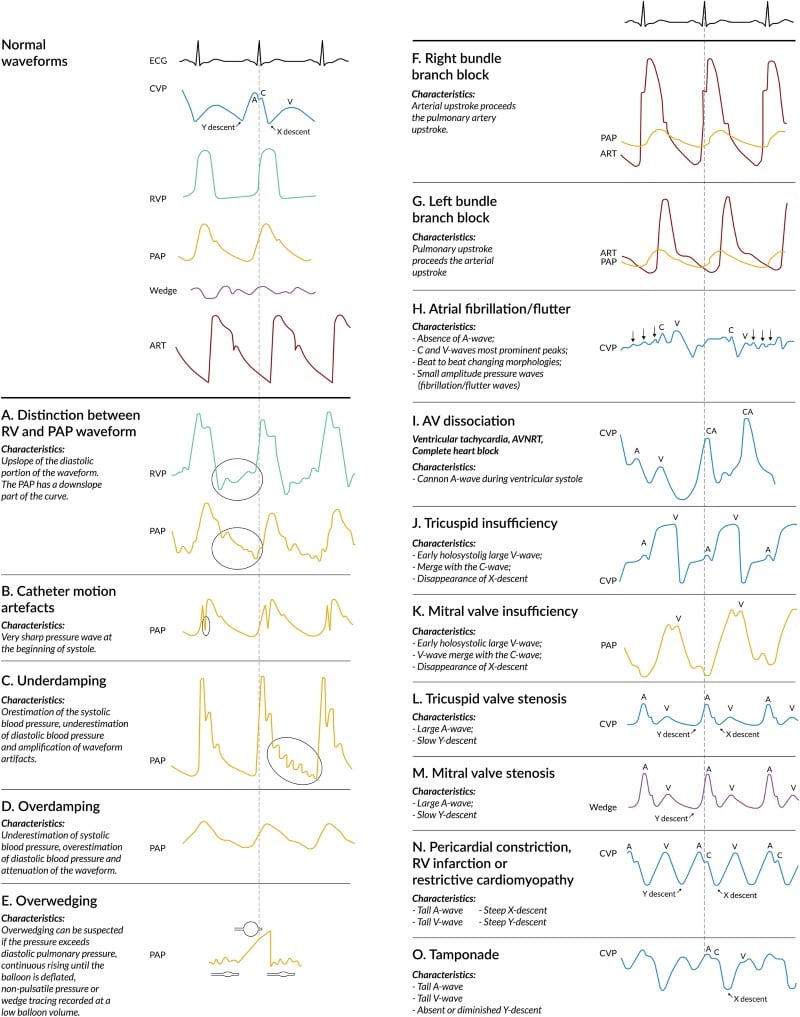
Figure 3. Abnormal waveforms. (Image from Bootsma et al., 2022; open-access article)6
CVP Waveform Abnormalities
Atrial fibrillation: Considering a-waves are comparable to p-waves on an EKG, if a patient has atrial fibrillation or atrial flutter, we won’t see clear a-waves in CVP waveform. There are also beat-to-beat shifts with the a-waves and they are smaller in amplitude. (Figure 3-H).
Pericardial constriction/Restrictive cardiomyopathy: In pericardial constriction, the CVP is elevated because the heart is not able to pump blood to the rest of the body secondary to elevated pressures. Therefore, the a-wave and v-wave will be elevated. There will also be a steep slope in the x-descent and y-descent. (Figure 3-N).
Tamponade: Tamponade is very similar to pericardial constriction, but the y-descent is absent or diminished. The PAP waveform is better at delineating between tamponade and pericardial restriction. (Figure 3-O).
Valve abnormalities: Valve stenosis – The a-wave will be large with a slow y-descent. This occurs because the pressure in the atrium increases and the blood has a more difficult time leaving the atrium secondary to valve stenosis. Therefore, the A wave is larger, and the y descent is slower. It will also increase the mean CVP. (Figure 3-L, 2-M)
Valve insufficiency: The A wave is small, the V-wave is large and merges with the C-wave, and lastly, the X-descent is missing. Since blood is coming back into the atrium during systole due to an incompetent valve, the V-wave becomes holosystolic and the C-wave merges with the V-wave. The x-descent disappears since the atrium is not able to relax. (Figure 3-J)
Pulmonary Artery Pressure Waveform Abnormalities
The Swan-Ganz catheter records oscillations in the blood pressure and displays them as peaks and troughs which we interpret as a systolic and diastolic pressure. Typically, there can be 1.5-2 oscillations. However, if there are more oscillations or less oscillations you should be concerned for underdamping or overdamping respectively.6
Underdamping: Occurs when there are more oscillations in the waveform. This is likely secondary to artifact or tachydysrhythmias.8 An underdamped system overestimates systolic blood pressure, underestimates diastolic blood pressure, and creates a wider pulse pressure (Figure 3-C). The MAP is not impacted.6,8
Overdamping: Occurs when there are fewer oscillations in the waveform. This can be caused by blood clots, obstruction of the pressure channel, or failure to remove air from the catheter or tubing (8). An overdamped system will cause an underestimation of systolic blood pressure, overestimation of diastolic blood pressure, and a narrowed pulse pressure (Figure 3-D). Similar to underdamping, the MAP is not affected.6,8
Pulmonary Artery Wedge Pressure Waveform Abnormalities
Wedging refers to balloon inflation within the pulmonary artery. You should see 2 clear positive and negative deflections in this waveform. If not, you should be concerned for overwedging or underwedging.
Overwedging: Occurs when the balloon inflation occludes the pulmonary artery wall, thereby preventing intravascular pressure measurements. If the wedge pressure is higher than the diastolic pulmonary pressure, the waveform is continuously rising, or the pressure is non-pulsatile.6 If this occurs, deflate the balloon and withdraw the catheter to a more proximal position for proper pressure measurements.
Underwedging: Occurs due to incomplete occlusion of the pulmonary artery branch. This will lead to overestimation of the PAWP.6
Thermodilution
PA catheters can also be used to measure cardiac output (CO) using the thermodilution technique. A thermistor that measures blood temperature is located at the catheter tip (within the pulmonary artery). The thermodilution technique involves injection of a cold saline solution into the right atrium (via the proximal port shown in Figure 1) and subsequent measurement of blood temperature in the pulmonary artery by the thermistor.10 As the cold saline mixes with the blood passing through the ventricle and into the pulmonary artery, blood temperature cools. How quickly the pulmonary artery blood cools is translated into a calculation of right ventricular cardiac output (higher cardiac output equates to faster flow, leading to more rapid cooling of blood in the pulmonary artery). This is performed several times at a consistent time point in the respiratory cycle (typically end expiration) to obtain an average thermodilution curve (Figure 4).
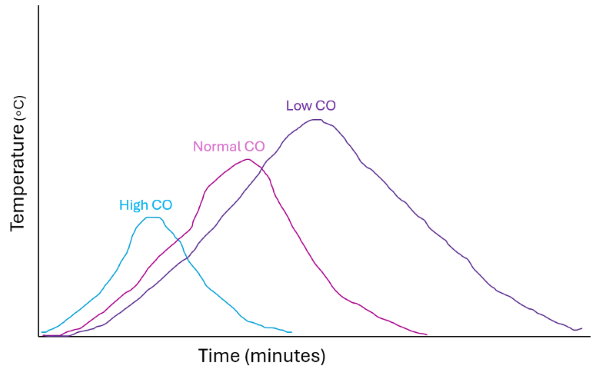
Figure 4. Thermodilution curve. High cardiac output will generate a shorter, steeper thermodilution curve as a result of rapid blood flow from the right ventricle to the pulmonary artery. Low cardiac output will generate a longer, slurred curve with a larger area under the curve (AUC). Abbreviations: CO, cardiac output.
Review of Measurements
|
Measurement |
Normal value (mm Hg) |
|
CVP |
0-10 |
|
RV Systolic Pressure |
15-28 |
|
RV Diastolic Pressure |
0 |
|
PA Systolic Pressure |
14-28 |
|
PA Diastolic Pressure |
6-16 |
|
Mean PAP |
10-22 |
|
PCWP |
5-12 |
Table 1. Normal hemodynamic measurements. Originated from Bootsma et al., 2022.6
Definitions for these measurements can be found in the “Normal Waveform” section. Based on these results, you can determine the type of shock a patient has, types of pulmonary arterial hypertension, cardiac output, cardiac index, etc.
Troubleshooting
If the pressure readings are inaccurate, the first step is to make sure that the system has the appropriate reference level and is appropriately zeroed. This is generally done in a semi-recumbent position at 30 degrees.7 Similar to an arterial line, a transducer is placed at the fourth intercostal space in the axillary line. The system is then opened to the air to establish atmospheric pressure as 0.11
If the catheter is zeroed, but is still showing inaccurate pressures, confirm the placement of the catheter. Placement should be confirmed at the time of insertion. This can be done if the catheter was placed under fluoroscopic guidance or by using a transesophageal echo.7
After zeroing and the catheter placement is confirmed, a "fast-flush" test is performed. A push of saline is pushed into the device, and it should cause a rapid upstroke in patients followed by a rapid downstroke in pressure. If there are increased oscillations, it is likely that the system is underdamped. If there are no oscillations, then the system is overdamped.7
Complications
During insertion of the central line preceding the PA catheter, there is a risk of pneumothorax or hemothorax. There is also a risk of infection, thromboembolism, and air embolism if air remains in the infusion ports prior to insertion. Lastly, there is the risk of atrial or ventricular arrhythmias which occur due to the catheter irritating the myocardial wall.3
Inflation of the balloon can also cause complications in the pulmonary artery. It has been associated with pulmonary artery perforation, rupture12 or a pseudoaneurysm formation.13 There can also be a pulmonary infarction if the balloon is inflated for a long period of time or if it migrates to distal pulmonary branches blocking off circulation.3
Take-Home Points
- A Pulmonary artery catheter is a useful tool in guiding management in complex hemodynamic states such as cardiogenic shock, right ventricular failure, and during complex cardiothoracic procedures.
- PACs allow accurate measurement of cardiac function and can guide resuscitation management.
- PACs provide accurate measurements of the pressure within the right atria, right ventricle and the left ventricle, which can be obtained by obtaining a wedge pressure.
- PACs are placed via Seldinger technique, advancing the catheter until the appropriate wave form is present to confirm that the catheter is within the pulmonary artery. They are zeroed similarly to an arterial line.
- When floating a PAC, ensure that the balloon is fully inflated each time the catheter is advanced and fully deflated each time it is withdrawn.
- Changes in pressure waveforms can be indicative of specific cardiac pathologies including restrictive cardiomyopathy, cardiac tamponade, and valvular abnormalities.
- Absolute contraindications to PACs include significant RV pathology such as tumors, right-sided endocarditis, and RVADs. Complications are similar to those associated with central line placement, as well as pulmonary artery rupture or pseudoaneurysm formation.
References
- Thakkar AB, Desai SP. Swan, Ganz, and their catheter: its evolution over the past half century. Ann Int Med. 2018;169:636-642.
- Chatterjee K. The Swan-Ganz catheters: past, present, and future. A viewpoint. [published correction appears in Circulation. 2009;119(21):e548]. Circulation. 2009;119(1):147-152.
- Rodriguez Ziccardi M, Khalid N. Pulmonary Artery Catheterization. [Updated 2023 Aug 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482170/.
- Nair R, Lamaa N. Pulmonary Capillary Wedge Pressure. [Updated 2023 Apr 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557748/.
- Kelly CR, Rabbani LE. Pulmonary-Artery Catheterization. N Eng J Med. 2013;369(25):e35.
- Bootsma IT, Boerma EC, de Lange F, Scheeren TWL. The contemporary pulmonary artery catheter. Part 1: placement and waveform analysis. J Clin Monit Comput. 2022;36(1):5-15.
- Fleitman J. Pulmonary artery catheterization: Interpretation of hemodynamic values and waveforms in adults. In: UpToDate, Connor RF (Ed), Wolters Kluwer. (Accessed on March 31, 2025.)
- Rezaie S. Damping and Arterial Lines. REBEL EM blog, July 4, 2022.
- Headley J. Pulmonary Artery Catheters and Assessment of Pulmonary Artery Wedge Pressure. Crit Care Nurse. 2014; 34(4):85-86.
- Klabunde R. Measurement of Cardiac Output. In: Cardiovascular Physiology Concepts, 3rd ed. Updated Jan 23, 2023. Accessed Apr 26, 2025. Available from: https://cvphysiology.com/cardiac-function/cf021.
- Weinhouse, GL. Pulmonary artery catheters; Insertion technique in adults. In: UpToDate, Connor RF (Ed), Wolters Kluwer. (Accessed on March 31, 2025.)
- Bossert T, Gummert JF, Bittner HB, Barten M, Walther T, Falk V, Mohr FW. Swan-Ganz catheter-induced severe complications in cardiac surgery: right ventricular perforation, knotting, and rupture of a pulmonary artery. J Card Surg. 2006;21(3):292-295.
- Nellaiyappan M, Omar HR, Justiz R, Sprenker C, Camporesi EM, Mangar D. Pulmonary artery pseudoaneurysm after Swan-Ganz catheterization: a case presentation and review of literature. Eur Heart J Acute Cardiovasc Care. 2014;3(3):281-288.