Phenibut, first introduced in Russia in the 1960s, has recently grown in popularity in the United States for its anxiolytic properties and its easy availability without a prescription.
After listing a few common home medications, a young, reasonably healthy patient recently reported that he used a supplement called phenibut for anxiety. During the interview, he was quite anxious with pressured speech. A few minutes later, he became acutely hypotensive and unresponsive. He received a standard workup for altered mental status, which was essentially negative aside from marijuana on a drug screen. Revisiting his medication list, a quick search of phenibut showed that it was not a supplement but a resurrected Russian medication now available over the counter.
Phenibut: What is it?
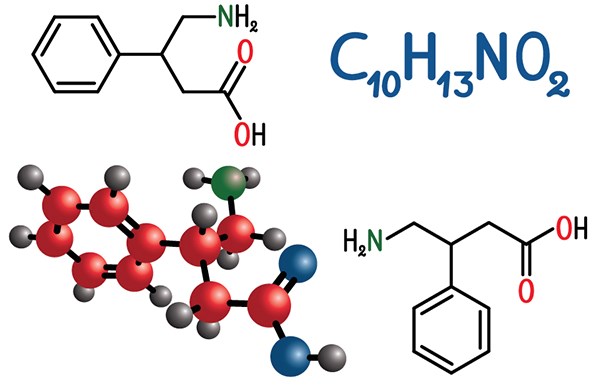
Phenibut (β-phenyl-γ-aminobutyric acid) is a GABA analogue that was first introduced in Russia in the 1960s. Its primary use in Russia has been as an anxiolytic and nootropic medication. The toxidrome of phenibut most closely resembles that of medications in the benzodiazepine class, but its effects are poorly studied apart from limited case reports.1
What does an overdose look like?
All documented case reports demonstrate somnolence or unresponsiveness as the primary presenting symptom with otherwise unremarkable laboratory workup. Case reports from Australia and more recently the U.S. have demonstrated significant toxicity and withdrawal symptoms, some of which have required intubation and ICU care.2-6
Learning from Australians—something we're all familiar with
Phenibut came to media attention in Australia following a well-publicized phenibut overdose in seven college students. In February 2018, the Australian Department of Health made phenibut a Schedule 9 substance, citing “reports of anxiety, insomnia, hypertension, hyperhidrosis, psychosis, tachycardia, widening of QRS complex, as well as CNS depression, delirium, seizures – potentially requiring intubation and ventilation.”7
How does it work?
Phenibut’s clinical effects may be better understood in light of two well-studied medication classes: benzodiazepines and anti-spasmodics.
Clinical effects similar to benzodiazepines
Both benzodiazepines and phenibut exert their effects by activating GABA receptors in the central nervous system, which results in the anxiolytic effects experienced with both medications. Phenibut is identical to GABA with the addition of a benzene ring. This allows it to cross the blood brain barrier more easily and bind to GABAB receptors in the central nervous system.1
Structurally similar to baclofen
Phenibut’s structure most closely resembles baclofen, another GABA analog. Baclofen has been used to treat muscle spasticity, and despite its similar structure, does not have significant anti-anxiety effects. Baclofen has poor crossing of the blood brain barrier due to an additional chloride moiety which makes its crossing stereoselective.8 This may be why baclofen does not have the same marked anxiolysis that phenibut has, but still may have neurotoxicity in high doses. Phenibut is able to cross easily, so it is able to have effects in the central nervous system.
Why are Phenibut overdoses on the rise?
Phenibut has recently grown in popularity in the United States for its anxiolytic properties and its easy availability without a prescription. Tolerance has been noted to develop quite quickly, and this leads to escalation of the dose to achieve the desired anxiolytic effects.9,10 This gives the drug significant abuse potential and increases the risk of toxicity from unintentional overdose and withdrawal. Additionally, it has been demonstrated that patients may experience significant withdrawal symptoms, including agitation and even psychosis.9,10
How can a phenibut overdose be treated in the ED?
With the information currently available, Phenibut overdoses or phenibut withdrawal should be treated the same way that benzodiazepine overdose or withdrawal is treated--typically with supportive measures. Depending on the severity of symptoms and any changes in vital signs, this may range from observation alone to intubation and monitoring in the intensive care unit. The half-life of phenibut in plasma is 5.3 hours.1 In most case reports, patients have been admitted to the intensive care unit for monitoring.
Can phenibut be detected on laboratory studies?
Two case reports have confirmed the diagnosis using gas chromatography-mass spectroscopy, but the diagnosis in the ED must typically be made clinically, as phenibut is not detected in commercially available urine drug immunoassays.2,11 The benzene ring of phenibut may interfere with methamphetamine testing on urine drug screen, so an unreportable methamphetamine screen might hint at the diagnosis.
Be wary of supplements
Phenibut is a controlled substance internationally, but available in the U.S. online for around $20. Patients are frequently unaware of the dangerous implications of supplements purchased online or over the counter. For medications and supplements not controlled by the Food and Drug Administration, consumers frequently rely on anecdotal online reviews and clever marketing. Many young patients do not follow with primary care doctors and instead self-medicate for many physical or mental conditions. For a young patient with anxiety, this will seem like an easy solution, and it may alleviate their symptoms. However, there is a reason that it has not been approved by the FDA for use as a medication in the U.S.--development of rapid tolerance makes it a poor choice for any long-term applications, especially when superior medications are available. In the U.S., over-the-counter supplements are commonplace, but in the emergency department we must be increasingly alert and aware of those supplements which are likely to cause clinical effects.
Back to the patient
After an unremarkable workup and fluctuating responsiveness in the ED, he was admitted to the intensive care unit, treated supportively, and able to be safely discharged home two days later after making a full recovery.
References
1. Lapin I. Phenibut (beta-phenyl-GABA) a tranquilizer and nootropic drug. CNS Drug Rev. 2001;7:471-481.
2. Sankary S, Canino P, Jackson J. Phenibut overdose. Am J Emerg Med. 2017;35(3):516.
3. O'Connell CW, Schneir AB, Hwang JQ, Cantrell FL. Phenibut, the appearance of another potentially dangerous substance in the United States. Am J Med. 2014;127:e3-e4.
4. Li CK, Sundararajan K. An uncommon case of phenibut toxicity in an intensive care unit. Int J Med Pharma Case Rep. 2015;5:1-6.
5. Downes MA, Berling IL, Mostafa A, Grice J, Roberts MS, Isbister GK. Acute behavioural disturbance associated with phenibut purchased via an internet supplier. Clin Toxicol. 2015;53:636-638.
6. Högberg L, Szabó I, Ruusa J. Psychotic symptoms during phenibut (beta-phenyl-gamma-aminobutyric acid) withdrawal. J Substance Use. 2013;18:335-338.
7. Australian Department of Health Therapeutic Goods Administration. Phenibut. https://www.tga.gov.au/book-page/33-phenibut.
8. van Bree JB, Heijligers-Feijen CD, de Boer AG, Danhof M, Breimer DD. Stereoselective transport of baclofen across the blood-brain barrier in rats as determined by the unit impulse response methodology. Pharm Res. 1991;8(2):259-262.
9. Ahuja T, Mgbako O, Katzman C, Grossman A. Phenibut (β-Phenyl-γ-aminobutyric Acid) Dependence and Management of Withdrawal: Emerging Nootropics of Abuse. Case Rep Psychiatry. 2018;2018:9864285.
10. Samokhvalov AV, Paton-Gay CL, Balchand K, Rehm J. Phenibut dependence. BMJ Case Rep. 2013;2013.
11. Wong A, Little M, Caldicott D, Easton C, Andres A, Greene SL. Analytically confirmed recreational use of phenibut (β-phenyl-γ-aminobutyric acid) bought over the internet. Clin Toxicol. 2015;53:783-784.