Clinical Presentation, Diagnosis
A patient in his 60s with a history of COPD, type 2 diabetes mellitus, hypertension, hyperlipidemia, and spinal stimulator presented to the emergency department for weakness. The patient’s family had found the patient on the floor, minimally responsive. When EMS arrived, he was not using his right side and had a leftward gaze. Vital signs were stable, he was afebrile, and BGL was normal.
The patient had been discharged 5 days earlier from a brief admission after being diagnosed with anemia and liver lesions that did not demonstrate neoplastic process on biopsy. A CT scan of the head at this encounter revealed a large, left-sided cerebellar mass with edema resulting in displacement of the fourth ventricle and hydrocephalus. Mannitol and dexamethasone were given in the ED, and neurosurgery was consulted. The patient’s mental status continued to deteriorate and he was intubated, allowing neurosurgery to place an EVD. The patient was admitted to the neuro ICU with initial considerations favoring subacute stroke vs. mass.
The patient was unable to have an MRI due to a spinal cord stimulator and had serial CT scans. He was taken to the OR 3 days later and found to have purulent drainage, making the diagnosis of a brain abscess. Cultures grew strep intermedius, and he was started on vancomycin, ceftriaxone, and metronidazole.

Image 1: Hospital day 1

Image 2: SP-craniotomy
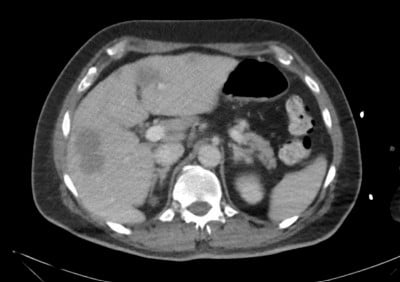
Image 3: Liver lesions, hospital day 2
Brain Abscess Review
Pathogenesis
The most common pathogenesis of bacterial brain abscesses is a result of contiguous spread, which makes up about 50% of all cases. The next most common cause is hematogenous spread, which represents about one-third of cases, and the remainder of cases remain unknown.1 Historically, case fatality rates had been as high as 40%, but over the past few decades we have seen drastic improvements to as low as 10% fatality. Full recovery has also increased from 33% to 70%.1 Immunocompromising conditions such as HIV can predispose patients to brain abscesses from not only bacterial sources, but also fungal and protozoan infections.2
Clinical Manifestations
Unfortunately, like with this patient, these infections can initially be difficult to diagnose, and the classic triad of headache, fever, and altered mental status are only present in about 20% of cases.1 Especially in abscesses near the brainstem or cerebellum, symptoms such as changes in gait, cranial-nerve palsies, or changes in mental status secondary to hydrocephalus can assist in diagnosis and work-up.3 Fever and other infectious symptoms can be present in patients who have hematogenous spread. With cerebellar abscesses specifically, 93% of cases in one study were secondary to odontogenic abscess spread.3
Diagnosis
Cranial imaging is the gold standard for diagnosing brain abscesses. Initially, CT imaging is likely to be performed to evaluate for hemorrhage, multiple lesions, masses, hydrocephalus, etc., but eventually MRI is preferred. Diffusion-weighted MRI has been shown to have a sensitivity and specificity of differentiating abscess from primary malignancy of 96% and 98%, respectively.4
Treatment
Treatment of brain abscesses consists primarily of neurosurgical intervention in conjunction with antibiotic therapy. Initial antibiotic treatment is broad and meant to cover the most common organisms including staphylococcus and streptococcus species but should be broadened out to cover opportunistic infections caused by HIV or other immunocompromised states when present.3,5 The abscess aspirate should be cultures following neurosurgical intervention to determine an organism and guide therapy.6
Case Resolution
The patient continued antibiotic therapy for about 2 months for his brain abscess as well as liver abscesses. He had a tracheostomy and peg tube placed while critically ill and was eventually able to be weaned off both of these. His hospital course was complicated by incidental bilateral pulmonary embolisms as well as NET found during PEG tube placement. He was able to be discharged just over 1 month following his presentation to the ED. He was readmitted 5 months later following a tonic-clonic seizure and was started on an AED.
Take-Home Points
- Brain abscesses can be difficult to diagnose and often mimic other intracranial pathology such as stroke or malignancy.
- These patients may not exhibit infectious symptoms such as fever, leukocytosis, etc.
- Keep this diagnosis in mind when initial imaging is unclear, especially in an immunocompromised patient who may need more specific antibiotics for opportunistic infections.
References
- Brouwer MC, Coutinho JM, van de Beek D. Clinical characteristics and outcome of brain abscess: systematic review and meta-analysis. Neurology. 2014 Mar 4;82(9):806-13. doi: 10.1212/WNL.0000000000000172. Epub 2014 Jan 29. PMID: 24477107.
- Tan IL, Smith BR, von Geldern G, Mateen FJ, McArthur JC. HIV-associated opportunistic infections of the CNS. Lancet Neurol. 2012 Jul;11(7):605-17. doi: 10.1016/S1474-4422(12)70098-4. PMID: 22710754.
- Shaw MD, Russell JA. Cerebellar abscess. A review of 47 cases. J Neurol Neurosurg Psychiatry. 1975 May;38(5):429-35. doi: 10.1136/jnnp.38.5.429. PMID: 1151412; PMCID: PMC491994.
- Reddy JS, Mishra AM, Behari S, Husain M, Gupta V, Rastogi M, Gupta RK. The role of diffusion-weighted imaging in the differential diagnosis of intracranial cystic mass lesions: a report of 147 lesions. Surg Neurol. 2006 Sep;66(3):246-50; discussion 250-1. doi: 10.1016/j.surneu.2006.03.032. PMID: 16935625.
- Schwartz S, Ruhnke M, Ribaud P, Corey L, Driscoll T, Cornely OA, Schuler U, Lutsar I, Troke P, Thiel E. Improved outcome in central nervous system aspergillosis, using voriconazole treatment. Blood. 2005 Oct 15;106(8):2641-5. doi: 10.1182/blood-2005-02-0733. Epub 2005 Jul 5. PMID: 15998833.
- Zumla A. Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Lancet Infect Dis. 2010 May;10(5):303–4. doi: 10.1016/S1473-3099(10)70089-X. Epub 2010 Apr 21. PMCID: PMC7128814.