Ch 10. Subspecialty: Nuclear Emergencies
Types of Radiation Exposure
- Radiation is the release of energy from atoms. It can be cate- gorized as non-ionizing or ionizing.
- Non-Ionizing: Low intensity and low frequency waveforms, such as microwaves and heat.
- Ionizing radiation is composed of particles and high frequency waveforms with sufficient energy to remove electrons from atoms.
- Alpha particle: 2 protons and 2 neutrons. High energy with low penetration. Travels only a few centimeters in air. Primary sources include uranium and plutonium. Main risk is inhalation injury or ingestion.
- Beta particle: Travels several meters. Penetrates several centimeters into tissue. Potential sources include Carbon-14, Iodine-131, Radium-226, Cobalt-60, Selenium-75. Hazardous as an external or internal contaminant.
- Neutron particle: Variable energy and penetration. Major source from fission reactions, such as nuclear weapons and power plants.
- May be absorbed by metal devices.
- Waveforms: Electromagnetic energy, such as x-ray and gamma rays, emitted from the cell nucleus. High energy and high penetration of tissue. Gamma emitters include Cobalt-60, Cesium-137, and Iridium-192. Large doses of whole body exposure can cause acute radiation sickness.
Detection
EMS detection of radiation can be accomplished by:
- Portable instruments: “Geiger counter” is the most commonly used.
- Personnel dosimeters: Worn on the anterior thorax. These instruments should be provided to all staff working in a potentially contaminated field.
First responders must consider that, in the post-9/11 era, any bombing could potentially be a “dirty bomb.”³ In addition, re- sponders should suspect potential radioactivity on any scene they see the trefoil, which is the international radiation symbol.⁵

En-Route Considerations
Responders should attempt to gather as much information as possible while traveling to an incident that could involve a ra- dioactive substance. A checklist to help determine initial actions should be developed and made available to all EMS personnel.
This checklist should include:¹
- Type and nature of the incident
- Radioactive substance name if known
- Name and age of victims
- Signs and symptoms experienced by patients
- Injuries sustained by patients
- Routes of exposure
- Length of exposure
In addition, communication should be established with local authorities, particularly police and fire.
On Scene
In general, the ambulance should park upwind, uphill, and at a safe distance from a potential radioactive site.1 Helicopters should not be used as the transport vehicle, because the draft wind can stir up radioactive particles. Scene safety takes priority in the emergency response to a radiologic event. The primary goal of first responders is to isolate the scene. NIOSH, OSHA, USCG, and EPA recommend dividing the incident area into 3 zones, establishing access control points, and delineating a con- tamination reduction corridor based on the military model.(1,2)
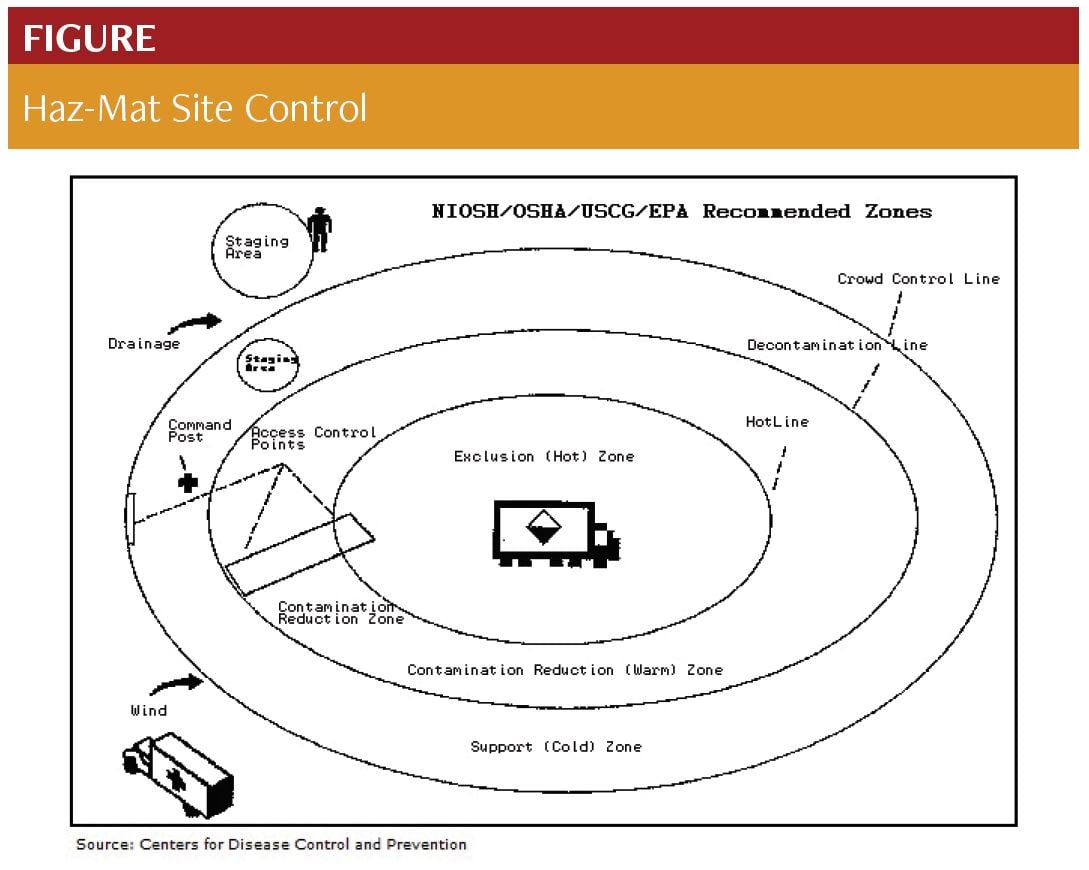
Exclusion (Hot) Zone: Encompasses all suspected hazardous material. The Gross Decontamination Phase and basic lifesaving measures such as airway and hemorrhage control occur in this zone.¹
Contamination Reduction (Warm) Zone: A safe distance from hot zone; may still have some contamination and PPE is still worn. Definitive decontamination occurs in this zone.¹
Support (Cold) Zone: Free of all hazardous contamination materials and includes the command and staging areas.
A quick scene assessment by trained personnel should deter- mine the nature of personal protective equipment (PPE) required in the Hot Zone.
Decontamination
In general, decontamination requires:
- A safe area.
- A method for washing off contaminants; typically large volumes of tepid water.
- A means of containing the rinsed and contaminated material, such as marked double plastic bags.
- PPE for providers.
- Disposable or cleanable equipment.
- This includes gross patient contamination and secondary/ definitive patient.
The Gross Decontamination phase includes the medical pro- vider’s primary assessment of ABCs, as well as the cutting away of clothing and jewelry once immediately life-threatening emergencies such as respiratory failure and hemorrhage are ad- dressed. Open wounds should be cleaned and then covered with a water repellant dressing. The patient should then be rinsed with tepid water from head to toe.
Definitive Decontamination occurs in the “warm” zone and involves making the patient as clean as possible before transfer- ring to the support zone and receiving facilities. Guidelines on duration of decontamination vary, but generally fall between 3-5 minutes, if not longer.4,6 If resources or time constraints do not allow for thorough cleansing, the patient should be cocooned in a blanket or sheet prior to transfer.
The removal of clothing and shoes will reduce external con- tamination by 70-90%. Thorough washing with soap and water will provide over 95% decontamination.
Treatment
EMS treatment of the victim of radiation contamination or exposure is no different from standard patients, with the ex- ception of the provider protecting oneself from contamination. The primary survey should be concurrent with the gross decontamination process. Secondary survey occurs when time allows. Treatment of airway emergencies follows standard protocols. Consider inhalation injury in anyone near blast sites. The majority of injuries resulting from a “dirty bomb” will be blast and ther- mal injuries.
Extensive burns require cleansing with saline or tepid water as part of decontamination. The patient should then be covered with sterile dressings and preferably transported to a burn cen- ter. If able, provide comfort with analgesics.⁸
Transport
No patient should be transported who, at a minimum, has not undergone gross decontamination.1 Make sure to contact the re- ceiving institution and ask for instructions for entering the hos- pital with a contaminated patient. The ambulance should park in a designated decontamination area. Upon release of the patient to the hospital, inquiries can be made as to where the ambulance can safely decontaminate and whether the institution has proto- cols and resources for this. The ambulance should not go back into service until deemed safely decontaminated by an adequately trained staff, such as a haz-mat team coordinator.
Resources
- Agency for Toxic Substances and Disease Registry. Managing Hazardous Material Incidents (MHMI). Volumes 1, 2 , and 3. Agency for Toxic Substances and Disease Registry (ATSDR). 2001. Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service
- Brennan R, Waeckerle J, Sharp T, et al. Chemical warfare agents: emergency medical and emergency public health issues. Ann Emerg Med. 1999;34(2):191-204.
- Broad W, Engelberg S, Glanz J. A Nation Challenged: The Threats; Assessing Risks, Chemical, Biological Even Nuclear. The New York Times; November 1, 2001.
- Burgess JL, Kirk M, Borron SW, et al. Emergency department hazardous materials protocol for contaminated patients. Ann Emerg Med. 1999;34(2):205-212.
- The Emergency Response Guidebook. A Guidebook for First Responders During the Initial Phase of a Dangerous Goods/Hazardous Materials Transportation Incident. 2012.
- Houston M, Hendrickson RG. Decontamination. Crit Care Clin. 2005;21(4):653-672.
- Radiation Emergency Assistance Center/Training Site (REAC/TS). http://www.orau. gov/reacts/default.htm
- Skorga P, Persell DJ, Arangie P, et al. Caring for Victims of Nuclear and Radiological Terrorism. The Nurse Practitioner. 2003;28(2):25-41.