Ch. 7 - Building Your ERAS Application
By now, you have started to consider the different types of EM residency programs available (Chapter 4), you have completed or scheduled your EM clerkships and USMLE exams (Chapters 3 and 5), and it’s time to understand how you actually go about applying to residency programs. There are several components of the application, and each will impact your competitiveness (Chapter 8).
The Electronic Residency Application Service
ERAS is a platform offered by the AAMC and used by most specialties for senior medical students applying for residency positions.1
The ERAS application helps you get a foot in the door with an interview invitation. In addition, it provides content, so residency program leaders can learn about you and help prompt interview discussion. Furthermore, the application helps guide the program director’s rank list.
How Do I Create an ERAS Account?
Registering for ERAS requires a “token” that will be provided to your medical school’s Dean’s office.
IMG Students: Visit ECFMG.org to obtain an ERAS token via the Online Applicant Status and Information Systems (OASIS) portal. Graduates of Canadian medical schools should visit CaRMS.ca for information how to register for ERAS.
Military Match: The military uses a separate application system through MODS (Medical Operational Data System); however, you must also apply through ERAS to be considered for civilian programs in case of deferment.
Know The Timeline
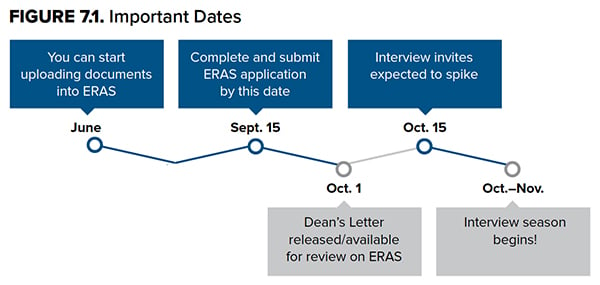
Keep key dates in mind when approaching the application process. The first is the date ERAS opens and you can begin editing your application and uploading documents. Historically the opening date was July 1; however, for the 2019 application cycle, ERAS opened earlier (June 7) so applicants could have more time to work on their application. Also new to the 2019 application cycle, ERAS began allowing students to start applying to ACGME-accredited programs in early September (Sept. 5).
Residency programs are granted access to applications and supporting documents beginning Sept. 15 at 9 a.m. ET. All applications submitted up to this point will be stamped with that date and time. The early submission window was created simply to avoid technical difficulties related to the huge volume of applications being submitted simultaneously. Submitting your application before Sept. 15 will help reduce the possibility of overwhelming the website, but it will not give you any advantage in terms of when programs will receive your application.
Stick to the Timeline!
Some program leadership may start looking at applications on Sept. 15 while others wait until Oct. 1 when the MSPE is available. However, it is imperative that you submit your application as close to Sept. 15 at 9 a.m. ET as possible. In a prior survey of PDs, only 15% of respondents stated that it was “highly likely” that an application would be reviewed if it were completed after the ERAS opening date.6
Regardless of when you apply, once you certify and submit your application, you will not be able to make changes other than on the Personal Information section and uploading additional letters. Consider assembling your application in June of your fourth year to avoid delays.
Military Match: The deadline for initial application to military programs through MODS is the second week of September, and supporting documents are typically due Oct. 15. Rank list is usually submitted around this time as well. Keep these military-specific deadlines in mind as you mustcomplete both MODS and ERAS simultaneously.
Latecomers: Don’t wait for rotations or letters. Submit your application on time. A program will wait for a letter, but they won’t wait for you.
The Components of ERAS
- Personal and biographic information
- Curriculum Vitae (education, experience, licensure, publications)
- Personal Statement
- Letter(s) of Recommendation
- USMLE transcript and/or COMLEX-USA transcript
- Medical Student Performance Evaluation (MSPE or “Dean’s Letter”)
- Medical school transcript
- Photo (optional)
Personal and Biographic Information
This section is where you enter your basic demographic and biographic information as well as military service obligations and whether or not you are couples matching. There is also a section for you to include your NRMP match ID, which you will get when you register for the NRMP Match. This is a separate process from creating and submitting your ERAS application. You must go to the NRMP website (www.nrmp.org) to register. Note that NRMP match ID registration does not open until Sept. 15 at 12 p.m. EST. You do NOT need this ID number in order to submit and certify your ERAS application, and you can add it later — so don’t wait for it.
Couples Match: Discuss with your advisors and partner if you will disclose your couples match status on ERAS. There are benefits and potential risks of doing so. You are not mandated to disclose. A handful of programs may want to avoid EM-EM couples. Additionally, if a partner is applying to a specialty that is not offered at the same institution, some PDs may not be aware of the non-EM training programs offered at hospitals nearby, leading them to think the interview may be low-yield.
Curriculum Vitae
The CV is simply a combination of several individual sections within ERAS that is compiled into a different format for readers in case they prefer to view the items in one document rather than on separate tabs within ERAS. These individual sections include Education (along with awards, membership in professional societies, languages spoken, hobbies/interests, and interruptions in medical training), Experience (research, work, and volunteer), Licensure (board scores, life support certifications, prior licensure information), and Publications.
While board scores, SLOEs, and medical transcripts provide objective data for residency program leadership, this section allows you to describe accomplishments outside of the classroom/wards, as well as to highlight personal qualities and attributes not captured elsewhere in the application. This section is often thought of as the “X-factor” of your application and helps reviewers gauge if you resonate with the program’s values. There is a real opportunity to stand out from other applicants; just listing your experiences does you a disservice. The application is much stronger if you include brief details of each activity to highlight your role and specific characteristics you developed through each experience. Demonstrate what you learned from each experience or how it made you a better person. Also, take advantage of the personal interests section. This is one of the few chances you will have to talk about yourself outside of medicine, and it’s frequently a great springboard for conversations during program interviews. A common pitfall in this section of the application is exaggerating the amount of time committed to each activity. Be truthful always.
At-Risk Candidates: Applicants with a history of felony or misdemeanor convictions will be required to disclose this. There will be a text-box to provide details. An applicant with this history is best served accepting responsibility, taking ownership of any mistakes, and demonstrating conscious changes for the better.
Latecomers: Include activities and accomplishments in other fields on your CV if they are substantial. Leadership, work, and research in other specialty areas may still be relevant. EM as a specialty requires a broad set of skills and interests.
Personal Statement
Personal statements can cause a high level of anxiety. How do you write a personal statement that captures your excitement as you apply to the field you want to practice? What is the role of the personal statement? How does it differ from other parts of your application? How much will it matter? A survey of EM residency directors showed the most influential components of residency applications are SLOEs, residency interviews, EM evaluations/grades, and clinical clerkship grades. The personal statement ranked below all of these components in importance.2 This is good news and bad news. It is unlikely a great personal statement will make up for an application that is otherwise poor, but sometimes a great personal statement can tip the scales in your favor.
So how do you write such a statement? The personal statement allows the residency selection committee to “meet” you before meeting face-to-face. Introduce yourself. Show (rather than tell) programs that you have the qualities to be a great resident by using examples from your previous experiences and achievements. Writing about how much you enjoy emergency medicine does not distinguish you from any other applicant; focus instead on what makes you unique. Describe the challenges you’ve faced to demonstrate your ability to persevere. Highlight how your previous experiences show your passions, values, and goals, and how you plan to channel your intelligence, creativity, and compassion into your career. Don’t go overboard by including examples from every previous experience; you will have a chance to talk about these in the experiences section. Choose a few examples that really highlight who you are and what you’re looking for in a residency. Committees want to know you will be a good fit with their program, so discuss what you are looking for in a residency program and what you want to gain from the next 3–4 years of your life. Make the personal statement personal.
Other essential facts that apply to all writing you are submitting apply here too.3 Edit your statement, put it away for a few days, then edit again with fresh eyes. Have those you trust read it as well. Take the recommendations with a grain of salt, but make sure you correct all spelling and grammar.
Although it is stressful, try to have some fun with the process. It is, by definition, the most personal part of the application. Allow yourself to reflect on what
makes you really you, and let that shine through.
Each statement is limited to 28,000 characters. There is no limit to the number of personal statements that can be created, and you can create program-specific personal statements (but be very careful not to send the wrong statement to the wrong program).
At-Risk Candidates: Applicants who have a facet of their application that is likely to be considered a red flag, such as a USMLE or course failure, a felony or misdemeanor conviction, an unaccounted for gap in their CV, etc., should use the personal statement to address these issues. This is likely the first place a reviewer will look for an explanation. If they do not find one, there is little incentive for them to go any further in considering you for an interview. Take ownership of your past and do not make excuses. Articulate how you have emerged from your challenges better equipped for a career in EM. And most important, have your advisor read your statement and give you feedback.
Latecomers: The personal statement may be a good place to explain how you came to EM as a specialty, but keep it succinct. Perhaps you had an “Aha moment,” so feel free to tell your story. Be sure your statement also shares experiences that convey the bigger picture of who you are and what you have to offer.
Dual Accreditation: Students applying to both EM and EM-combined programs or programs in a different specialty have the ability to upload multiple personal statements.
Letters of Recommendation
In Chapter 5: Applying for Away Rotations, it was discussed that the SLOE obtained at the end of each EM clerkship is the single most crucial component of your application and that 2 of them are recommended.2,4,5
ERAS allows you to submit a maximum of 4 LoRs to each program, but it is not necessary to upload 4. It is variable how many total letters a program will want before they consider a student’s application to be “complete enough” to offer an interview. It is important to know that after 4 LoRs are assigned to a program, you can no longer remove/add LoRs. Therefore, if you performed a later away rotation (September or later) but are counting on this rotation for a SLOE, it is important to leave a LoR spot open for this SLOE at the time of your initial application submission. Additional letters can be added as they become available, but do not delay submitting your applications while waiting for SLOEs to be uploaded.
Within ERAS, you must enter the names and titles of your letter writers, the specialty the letters will be used to apply to (emergency medicine), and whether or not you waive the right to view each LoR. In general, applicants normally waive the right to review their LoRs, allowing letter writers to provide an honest assessment. Once a LoR entry has been confirmed, you will be provided with a unique Letter ID and Letter Request Form that can be delivered to LoR authors by email directly from ERAS (with an optional custom message), or downloaded as a PDF, with instructions on how to upload your LoR.
While having both SLOEs uploaded by Sept. 15 can be to your advantage, it’s not a deal-breaker; many programs will still consider you with only one SLOE at the time of file review and interview offer — both will just need to be uploaded by time of applicant ranking. A third SLOE is rarely suggested but may be beneficial if you have red flags or had a challenging rotation.7,9 On EMRA Match,10 programs list how many SLOE(s) they expect to consider an applicant for an interview.
In addition to the 2 SLOEs recommended from your clerkship experiences, you can add LoRs from another EM faculty member with whom you have worked closely (for example, from a subspecialty rotation such as ultrasound, toxicology, EMS, etc.) or from a non-academic EM physician or a physician not in the specialty. However, it is important to note that SLOEs generated by EM experiences that are affiliated with a residency training program carry more credibility than a LoR from a non-academic EM physician or a physician not in the specialty.5
Latecomers: While studies show a LoR from a physician in a specialty other than EM carries less value than a SLOE, you may have a mentor or advisor from a different specialty who has worked closely with you.4 You can consider including a non-EM LoR if you had a strong relationship with the writer. Be sure to leave room in ERAS to upload 2 SLOEs before submitting your rank list.
USMLE or COMLEX Transcripts
Within ERAS, applicants must authorize the release of their Step scores from the NBME by entering their USMLE ID and paying a transcript fee. You can track the status of your transcript request by logging back into ERAS. If your Step 2 scores are not available at the time of your initial application, you must log back into this section of ERAS and select “Resend My Scores.”
Guidance about when to take USMLE Step 2 CK can be found in Chapter 3: Third Year and Planning for Fourth. Information about how your USMLE/COMLEX scores should influence your application strategy can be found in Chapter 8: Apply Smarter, Not Harder: Understand Your Competitiveness.
Osteopathic Students: You can upload COMLEX-USA transcripts, USMLE transcripts, or both. If uploading COMLEX-USA transcripts, you must authorize their release by entering your NBOME ID and paying a transcript fee, similar to the process for uploading USMLE scores. As mentioned in Chapter 2: The Preclinical Years, osteopathic students who take USMLE are more likely to match at ACGME programs. There is no direct conversion from COMLEX to USMLE scores for programs to compare you apples to apples. Refer to EMRA Match for programs that will accept COMLEX scores alone when helping make your application decisions (hint — it will not be a majority of programs!).16-18
IMG Students: USMLE transcripts for IMGs are released by ECFMG rather than NBME.
Medical Student Performance Evaluation (Dean’s Letter)
The MSPE is not a letter of recommendation, but rather a summary of your performance throughout medical school. The MSPE is a valuable part of your application because it gives a broader perspective of your four years of medical school. This evaluation emphasizes strong attributes demonstrated throughout your medical education, highlights your accomplishments during this time, and addresses any red flags or difficulties. It also provides a narrative to your clinical clerkship performances. The MSPE traditionally includes your rank compared to classmates, and this can help you gauge your competitiveness as an applicant; however, not all medical schools have a class ranking system. In this case, your school will indicate this in the MSPE. Check with your dean ahead of time to understand your institution’s process so you understand your own competitiveness. Training programs do not rely heavily on this component of the application when selecting applicants for interview, likely because it is released later than the rest of your residency application (Oct. 1 compared to Sept. 15). However, the MSPE is rated highly in importance when it comes to deciding how to rank applicants.2
At-Risk Candidates: Be familiar with your MSPE so you can address any red flags such as course failures or professionalism issues in your personal statement and during your interviews. Take ownership of the issues, reflect upon what you have learned, and be ready to explain the changes you have made to ensure that the past will not repeat itself during residency.
Latecomers: If you changed specialty choices, be sure to update your dean as soon as possible. They may choose to emphasize different aspects of your strengths or accomplishments as they relate to EM.
Medical School Transcript
This is simply a list of your preclinical and clerkship grades, which is released prior to the MSPE. Your MSPE will provide more detailed information about your clerkship performances. By the time you are putting together your ERAS application, there is not much you can do about any of this information. While basic sciences grades have been ranked lower in terms of importance to residency programs, performance in required third-year clerkships is cited as being heavily valued.2,4
Photo
This is optional, but the vast majority of applicants do upload a photo to ERAS. While your photo does not need to be from a professional photographer, you need to appear professional. No selfies!
The Bottom Line
- Be honest on your application; do not inflate your accomplishments or involvement in anything. Program directors also look for congruence. They want to make sure the person they interact with on the interview day is consistent with the person they see on paper.
- Anything on your application is fair game to be discussed further in an interview. If it is on your application, be prepared to talk about it!
- Spelling and grammar errors can be a kiss of death. Spend time making your application clear, crisp, and error-free. From the ERAS site, you can print your application to review for errors. Have friends, family, and mentors read over your application before you submit.
- Stick to the timeline. It is OK to not have 2 SLOEs uploaded by Sept. 15, but you must have your application submitted by this date. Do not submit late!




