Ch. 3 - Third Year and Planning for Fourth
The start of your third year marks the first major transition into regular clinical responsibilities. It is an exciting time! You are able to apply your basic science knowledge to clinical practice, participate as part of a health care team, and regularly spend time with patients. At the same time, your responsibility increases and more of your time is spent at the bedside rather than in the classroom. The way you learn may need to evolve, and your schedule will be more rigorous. Additionally, your performance in core rotations is a critical part of your residency application, so performing well is important. You will also be simultaneously planning your fourth year, which can be both exciting and stressful. What are the keys to success on rotation and advance planning?
Third Year
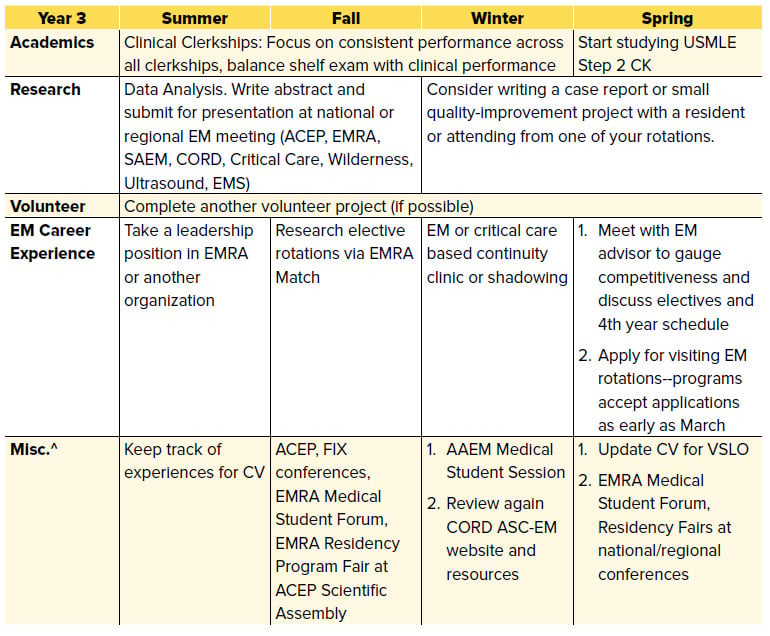
Figure 3.1 Important Time Frames in Third Year
Source: CORD ASC-EM Planner
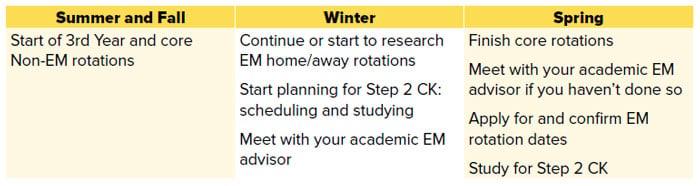
Military Match: If you are a military match candidate, the timeline is accelerated. Applicants should research rotations early (summer of third year) and plan to rotate much earlier than non-military peers. You will be applying for and scheduling rotations in the winter!
IMG Students: Ensure paperwork is completed in time to allow for U.S. rotations. Consider researching away rotations as early as possible (summer of third year) so you can apply preferentially to institutions that accept your visa.
Couples Match: Meet with your advisor (individually and as a couple) to discuss career goals and how to increase your competitiveness as a couple. Consider these questions: What does couples matching mean to you? What compromises are you willing to make? What compromises are you not willing to make?
Latecomers: If you are undecided about your specialty but considering EM, meet with an EM advisor early in third year to discuss your options.
Academic Performance in Core Clerkships
Performing well in your core clerkships is critical for a number of reasons.
Making the most of your rotations and performing at a high level will:
- Accelerate your Step 2 CK preparation
- Allow you to apply your knowledge to patient care during your EM rotation(s)
- Make you a more competitive applicant
Narrative comments from your evaluations and information about your performance relative to your peers will be included in the Dean’s letter. Per NRMP Match data from the 2018 PD Survey, 75% of PDs cited “Grades in required clerkships” as an important factor when selecting applicants to interview, with a mean importance rating of 3.9 out of 5.1 AOA and other honor society selection committees will also heavily consider your core clerkship performance. Lastly, your grades will impact your final class rank. One recent study found that EM rotation performance and AOA designation were predictors of top performance in residency.2 Additionally, EM rotation grades have been shown to correlate with rank list position.3
What does all of this really mean?
It means preparation for Step 2 and your EM rotations begins now, with your core clerkships. With each rotation you are building your knowledge base and residency application.
At-Risk Candidates: Failing a clerkship is a major red flag. On a recent CORD ASC-EM survey of EM educators, nearly all programs reported “rarely or never” interviewing applicants with a clinical course failure.4 A clerkship failure should prompt consideration of a non-EM backup plan and a meeting with your academic EM advisor. Alternatively, performing at a high level on clerkships can help mitigate the effect of a low USMLE Step 1 score.
Core Clerkship Pearls
Set yourself up for success on your core rotations — because all of them will ultimately help you be a better emergency physician. First, you can ask peers what worked well for them. What books did they read? Did they use any other resources? Next, make sure you review the syllabus and grading criteria. If a large part of your grade is exam performance, then creating a study plan for that rotation is important. And finally, be sure to ask for feedback from faculty and the clerkship director so you can identify areas for improvement early. Clerkship directors can help you come up with a plan to address these areas.
Table 3.1 Core Clerkship Pearls
Surgery — Success is all about dedication and preparation. Arrive early to pre-round, take time to “own” your personal patients, and absorb all you can about post-op care. Don’t avoid the OR; there you’ll learn valuable lessons on procedures (chest tubes, central lines, tracheostomies, etc.). Learning how to tie sutures is also essential. Examine any patient who is presenting for emergency surgery, as learning how to recognize an acute abdomen is a critical skill.
OB/GYN — You will deliver babies in the ED! Make every effort to get hands-on practice while on rotation. Pay particular attention to the techniques used in difficult deliveries (like shoulder dystocias). Also, practice reading fetal monitoring strips every day, as this is a skill commonly tested on your shelf exam. Ask if you are able to perform cervical checks during labor to start to get a sense of degree of dilation and understand the various stages of labor. Being sensitive to gynecologic complaints and expertly and gently performing a pelvic exam is an essential skill in the ED. Lastly, participate in the care of patients with preeclampsia or post-partum patients with complications or breastfeeding concerns — these patients often present to the ED after-hours.
Psychiatry — EM physicians care for patients with a variety of mental health complaints, and many of these patients have limited access to care. Learning how to help patients find community resources is key. Also, learning how to identify those in acute psychosis or with a true psychiatric emergency is critical. While rotating, try to become an expert in psychiatric medications, their dosing, interactions, and long-term and life-threatening side-effects.
Pediatrics — Although there are many things to memorize during your pediatric rotation (such as developmental milestones and immunization schedules), there are also EM-specific pearls. Learn the basics such as normal and abnormal vitals, how to properly suction an infant or toddler, and how to counsel families on safe-sleep habits. Take time to learn the basic treatment regimens for asthma, congenital abnormalities and their physiology, as well as changing physical exams at different ages.
Family Medicine/Internal Medicine — Understanding the hospital course and basic disease processes for the most common illnesses is critical. During your IM rotation it is especially important for you to take responsibility for your patients. Know their labs from 3 days ago, their vitals for the past 24–48 hours, and most important, ask the nursing staff how they are doing. Your IM rotation hinges on collaboration between you and the entire health care team. Family medicine rotations vary at different institutions. While rotating, try to become an expert in antihypertensive and diabetes medications, including their indications, dosing, interactions, and side effects.
Dean’s Letter/Medical Student Performance Evaluation
The MSPE is an aggregation of all of your medical school accomplishments and is compiled by your home institution. This letter places a heavy emphasis on your core clerkship performance and feedback, discusses your background, preclinical performance, and highlights any service work or publications you may have. Core clerkship performance is critical, with many MSPEs providing a visual representation of your performance compared with your peers (typically a series of bar graphs or charts). According to the 2018 NRMP survey, 84% of program directors cited the MSPE as an important factor when selecting applicants to interview, with a mean importance rating of 3.3 out of 5.1 Be aware of the content of your MSPE, because below-average performance or potentially negative comments could be seen as a red flag and should be discussed early with your academic EM advisor.
Planning for Your Emergency Medicine Clerkships
As an EM-bound student you should complete two EM rotations so you have two letters of recommendation (in EM we refer to these letters as SLOEs, Standardized Letters of Evaluation; see Chapter 6: Crush Your EM Clerkships, Secure Your SLOEs). While most required EM rotations are during fourth year, some EM rotations are offered during third year. Also, some schools with a required fourth-year EM rotation may allow students to rotate early (as an M3) if they have met the prerequisites. The experience gained on an EM rotation during the third year of medical school varies based on school, program, and timing. For example, if you rotate in the last month or block of M3, after all core rotations, that is much different than rotating in November of M3 before your surgery and pediatric rotations.
If your school offers or requires a third-year EM rotation, or permits you to schedule the M4 rotation as an M3, find out if they will write a SLOE. Some institutions will not provide a SLOE for M3s. Moreover, if a SLOE is an option, be sure to ask if the SLOE will compare you to other M3s or to the M4 cohort — the added experience, confidence, and clinical competence of the M4 group may diminish your evaluation. An experienced EM advisor can help answer some of these nuanced questions as each individual students’ circumstances are unique.
Ideally, you will complete your home institution (“home EM”) rotation as early as possible in order to get your feet wet before your away EM rotation. Unfortunately, EM is not a required rotation at all medical schools. If you do not have a home EM rotation with an ACGME-affiliated residency program, your only options will be away rotations. Late fall and early winter of your third year is the best time to start researching away emergency medicine rotations. EMRA Match is a great place to start when researching programs.5
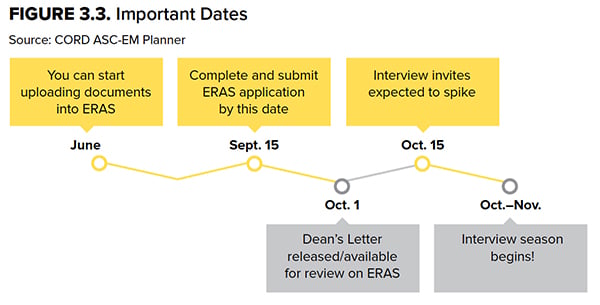
There is more than one method for you to apply for away rotations. The most critical thing is that you have at least 1 EM rotation completed before Sept. 15. (See Chapter 5 for more detailed information.)
Military Match: The timeline is accelerated. Applicants should research rotations early and plan to rotate as early as January of M3. Military rotations are set up by contacting the program directly via email.
Osteopathic and IMG Students: Be aware that your school may not have a home rotation so you must spend time researching academic programs with a history of accepting osteopathic and IMG applicants — EMRA Match can help with this.
Latecomers: Work with your EM advisor or clerkship director if you are having difficulty scheduling rotations. They can be an invaluable resource of experience and connections.
Fourth Year
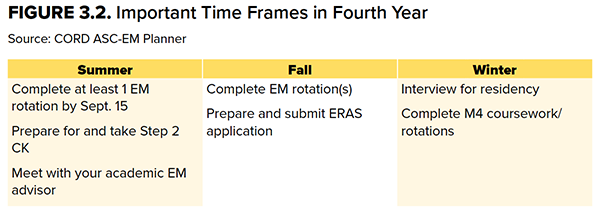
IMG and At-Risk Candidates: These applicants are encouraged to have 2 (as opposed to a minimum of 1) rotations completed early so that both SLOEs are in ERAS on opening day, or on/before the release date of the MSPE. According to a recent CORD ASC-EM survey, program leaders responsible for interviewing applicants recommend 2–3 SLOEs for IMG applicants.4
Military Match: The timeline is accelerated. The match takes place in December of fourth year. Apply and be prepared to interview at civilian programs in late December/early January in case you don’t match into a military program.
Latecomers: Even if you do not have a completed SLOE by opening day, do not delay in submitting your ERAS application. Only 15% of programs reported that it was “highly likely” that an application would be reviewed if it were completed after the ERAS opening date in September.11
USMLE Step 2 CK
Residency programs are evaluated on the rate at which their graduates pass the boards when they finish residency. It has been demonstrated for many specialties, including EM, that not passing the USMLE or COMLEX is a strong predictor of struggling to pass later exams. This correlation leads program directors to worry about applicants who struggle on these types of knowledge assessments. According to the 2018 NRMP PD survey, 86% of respondents listed USMLE Step 2 CK (and COMLEX Level 2CE scores) as a factor in offering interviews.1 Further, USMLE Step 2 CK scores were given a mean importance rating of 3.9 out of 5 (compared to 3.8 for USMLE Step 1). Because of its clinical focus, USMLE Step 2 is often considered to be at least equally important as USMLE Step 1.1,4 The bottom line is USMLE Step 2 CK performance is very important — your work is not done after USMLE Step 1!
Preparing for USMLE Step 2 CK begins during preclinical courses and spans all of your core clinical clerkships. Your daily efforts to make the most of your rotations and master the learning objectives will save you time in the long run. In considering Step 2 preparation, take some time to reflect on your USMLE Step 1 and clerkship exam performances: What worked well (or not)? What were your lessons learned? If you underperformed, make sure you have met with an advisor and/or consulted with your office of student affairs and come up with a plan to improve. Perhaps you need additional time in the form of a study month.
Students interested in matching into emergency medicine should take into account their USMLE Step 1 scores when deciding when to sit for USMLE Step 2 CK. Program directors may send interview invitations when applicants present an acceptable Step 1 score in conjunction with a robust application, despite not reporting a Step 2 CK score. Per NRMP data, 51% of programs do not require
Step 2 CK scores when deciding whom to interview.1 However, that means 49% do put some weight on this exam prior to granting an interview. Also, keep in mind that as you progress through fourth year, it could be more difficult to find time to study during away rotations and preparing your application.
If your Step 1 score is less desirable, it is recommended you attempt to bolster your application by taking Step 2 CK early (end of June or mid-July) so your scores are available for release to programs when ERAS opens on September 15. A significant improvement between Step 1 and Step 2 CK scores can help compensate for a lower Step 1 score. Most programs will require a Step 2 CK and Step 2 CS score prior to the rank list deadline.2 The average USMLE Step 1 score for unmatched applicants is 220.6 Additionally, the median Step 1 score below which programs generally do not grant interviews is around 210.1
As such, if you scored < 220 on Step 1, it is important to take Step 2 CK early.
Latecomers: Prioritize getting your first SLOE over taking Step 2 CK early. Both are important, but studies show the SLOE is more important in offering interviews.1, 3, 9-11
In general, it’s probably best to allow yourself time to focus on Step 2 and EM rotations independently. However, since there is significant overlap in the time period for completion of each, this may not be possible. Your school may have deadlines that mandate a completion date during a SLOE-granting EM rotation. For those who feel a dedicated study month (or 2 weeks) is needed this should be done only if timing allows for scheduling at least one EM rotation over the summer months. Remember your goal is to have at least 1 SLOE, but preferably 2, uploaded to ERAS by opening day.
Osteopathic Students: As there is no reliable score conversion from COMLEX to USMLE, it is strongly recommended that if you have not taken USMLE Step 1, you do take USMLE Step 2 CK early so your score is available when ERAS opens. This allows you to be compared apples-to-apples to your allopathic counterparts.7,8
Fourth Year Coursework
EM rotations take an average of 2 months. Your school may have required coursework, but students are often able to enroll in electives with flexible scheduling or take time off for interviews, etc. Because of the volume of interviews conducted in November and December, many students take time off during these months.1 According to the 2018 PD survey for the 2017–2018 interview season (Figure 3.4), the majority of interview invites were sent in October (60%) and November (21%), and interviews were conducted in October (10%), November (36%), December (34%), and January (18%).1
Figure 3.4 EM Program Interview Activities (n=84)
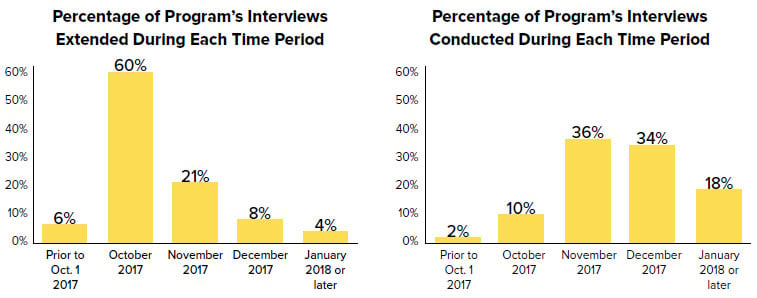
Copyright 2018 National Resident Matching Program. All rights reserved. Reprinted with permission. Permission to use, copy, and/or distribute any documentation and/or related images from NRMP publications shall be expressly obtained from NRMP.
Speak with your advisor or upper-year mentors who have gone through the specific coursework at your school to determine which electives are best for interview season in terms of flexibility for traveling and interviewing.
For any rotations during interview season, be sure to communicate with as much advance notice as possible regarding your interview schedule and travel requirements. Most courses or rotations have attendance requirements — so
keep this in mind. After you have completed your two EM rotations (home and away), consider broadening your coursework. As an EM physician, you will need to draw upon a broad skill set during your career. Through EM and non-EM electives you can build important skills.
EM Subspecialty Electives
In order to further explore your interests in the field of EM, consider an elective in a related area. There are several clerkships on VSLO in EM specialty areas including ultrasound, pediatric EM, toxicology, EMS, wilderness medicine, etc. Such rotations will help you expand your knowledge base and help you to get to know another program’s faculty and residents. It can also open your eyes to the versatility of a career in EM and help build your excitement for residency and beyond. While subspecialty rotations can sometimes provide a letter of recommendation, these letters are not given the same weight as a traditional SLOE because they reflect your performance in a narrow area within EM.
IMG Students and Latecomers: For applicants struggling to get 1–2 (or any) rotations that can provide a traditional group SLOE, an EM subspecialty elective may be the next best option.
Non-EM Electives
Ophthalmology
Eye complaints in the ED can be challenging for a number of reasons. Consider an ophthalmology rotation in order to become proficient at slit lamp examinations. Eye foreign bodies, ocular trauma, and vision loss complaints all warrant a good slit lamp exam. Additionally, learning how use fluorescein and measure intraocular pressure will certainly put you a step ahead as an intern.
Orthopedics
Performing a solid musculoskeletal exam as well as recognizing and reducing fractures and dislocations are crucial skills for any emergency physician. A rotation in ortho can also help you communicate effectively with your consultants in the department. Learning fracture types (Smith fracture vs. Colles fracture, etc.), nomenclature of specific bony areas, and key information for your consultant will make all of your interactions with orthopedics so much smoother. Make sure to also absorb all you can about splinting and casting! Our orthopedic colleagues have a wealth of information on the best ways to immobilize fractures and are usually very willing to impart that knowledge to you.
Dermatology
Take this opportunity to brush up on life-threatening rashes and recognizing lesions that may be indicative of serious diseases. Ask about outpatient medical management of common rashes and skin complaints and try to learn what needs emergent consultation vs. close follow-up.
Pulmonology
Working with a pulmonologist can provide fascinating insight into what happens to our respiratory distress patients after they are admitted. Learning about how to work a ventilator and set/adjust ventilator settings is a critical skill and cannot be overestimated. Be sure to observe a bronchoscopy whenever possible to gain a better understanding of the respiratory tree and the extensive sequelae of lung diseases. Pay particular attention to the medication and homecare of patients so you can help counsel your patients who have frequent visits for COPD or asthma exacerbations.
Critical Care
ICU experiences can provide opportunities to learn new procedural skills such as placing arterial lines or central lines. Managing patients on ventilators and various medication drips is a key skill for EM physicians. You can learn about ICU admission criteria and the care and treatment of patients with conditions commonly encountered in the ED such as sepsis, multisystem trauma, stroke, etc.
The Human Side of Medicine
The medical knowledge and clinical skills needed for EM are extensive, but communication, professionalism, and interpersonal skills will also be crucial in your career. They will likely contribute to your overall career satisfaction and even longevity. Take advantage of courses with focus on palliative care, difficult discussions, or even how to be a better educator. This will make you a stronger EM physician, respected colleague, and patient advocate.
Table 3.2. Timing of Courses, Clerkships, and Activities
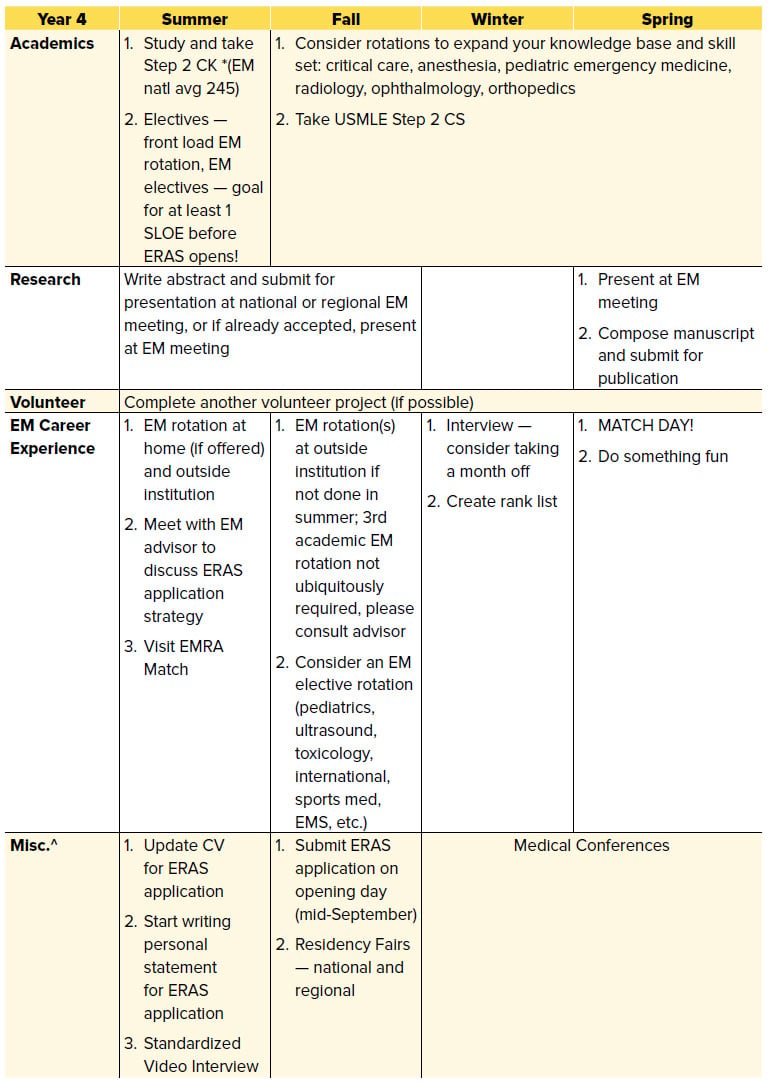
*All National Averages are based on the 2016–2017 first year EM resident. Available at https://www.aamc.org/data/484714/report-on-residents-2017-b1table.html. There is a large standard deviation, with some applicants having no research experience or publications. Numbers indicate all experiences over a 4-year medical school career.
^Conferences may offer numerous opportunities for students considering a career in EM; attendance is not required or considered a factor that influences a student’s potential to match in EM.'
THE BOTTOM LINE
- Core clerkships are critical in helping you with develop the knowledge and skills to succeed in emergency medicine and do well on USMLE Step 2; in addition, your performance will be highlighted in your MSPE and is important to EM PDs.
- Begin planning your fourth year early. This includes researching EM electives and brainstorming a strategy to prepare a complete ERAS application (when will you take Step 2? How many EM rotations do you need to complete before Sept. 15?).
- If you do not have an EM advisor now is the time to find one. An academic EM advisor can provide critical guidance on fourth-year planning.




