Ch. 12 - What If I Don't Match
So, you didn’t match. We are so sorry. We are hoping our words of wisdom can assist you in achieving success, whatever that may mean to you at this stage. As you reflect, it is important that you understand why you didn’t match; only with an honest appraisal of why you were unsuccessful can you plan your best approach to the SOAP, reapplication, or alternative career trajectory.
If you are reading this as someone who thinks you may be an at-risk applicant to not match, then you are one step ahead! Meet with an academic EM advisor now to discuss proactive strategies.
Why Are You Here?
Before you can form a plan to move forward, you need to know why you didn’t match. External evaluation should be a requisite portion of your application review. Any faculty member who told you that not matching would be a possibility is likely a good source (they were right). Your student affairs dean is another good resource, and a sympathetic program director can be a wonderful additional source of information.
Program type and number: Did you apply to the right number and type of programs?
You are assessed on two elements for matching: your paper application and your interviews. If you had an appropriate number of interviews (at least 10), it is probable that you had deficiencies in interviewing, and significant interview practice or attending an interview course should help.
If you did not get a reasonable number of interviews, either you did not apply to enough of the right programs, or something in your paper application is limiting you.
Evaluate the 5 elements of your application to find weak spots that may have caused you to not match. (Revisit Chapter 8: Understanding Your Competitiveness: Apply Smarter, Not Harder.)
- Step Scores: The average Step 1 score for matching EM students is 233; for Step 2 CK, it’s 247.1 Substantially lower scores are likely a barrier to getting interviews. If you did not take the USMLE or did not take Step 2 by mid-September, your application may not have been reviewed at all. Unfortunately, it is difficult to overcome this hurdle — the one method that can prove clinical acumen is to do well on additional rotations. Sometimes, you can delay medical school graduation to do additional rotations or do them in late winter/early spring before you graduate, but each rotation is serving you only at that institution, as additional SLOEs are unlikely to make a difference for getting you past the Step 1 hurdle. Similarly, applying to appropriate programs is crucial with a low Step score.
- ERAS Application: Red flags on the ERAS application include felony convictions, a dearth of involvement in any other activities, wildly unbelievable statements (such as 120 hours per week on a project) or inappropriate statements about activities, and leaves of absence without explanations.2
- Personal Statement: It is rare this makes a substantial difference, but grammatical errors, a statement shorter than three-quarters of a page, or inappropriate comments in your personal statement all can serve as barriers to getting an interview.
- LoRs (including SLOEs): This could be your blindside reason for not matching. SLOEs with comments such as “disinterested” or “confrontational” are barriers to matching. However, students are not able to see their SLOEs, so how can you know if a LoR or a SLOE is what caused you to not match? SLOEs are reflective of grades and comments received during a rotation, so low scores or less than enthusiastic comments are indications that a specific SLOE may not be the one to use.3 Ask your advisor or a sympathetic PD to review your letters and provide guidance about which letters they would recommend you make use of moving forward.
- MSPE: Most medical schools allow you to see your MSPE; the significant red flags within an MSPE are either in professionalism, time off, negative comments from clinical rotations, or low quartile ranking. Professionalism issues must be addressed in a personal statement, as they remain the largest red flag in an application. As MSPEs are finalized and follow you, other elements of the application must address any MSPE deficiencies.
SOAP
The Supplemental Offer and Acceptance Program occurs during Match Week to match unfilled spots with unmatched applicants. This is facilitated via ERAS and is a binding contract, just like the standard match.
You find out on Monday of Match Week at 11 a.m. ET whether you matched. An electronic list of unfilled programs who chose to participate in SOAP is available at that time. If you did not match, then at 2 p.m. Monday you can begin applying to programs in any unfilled specialty. Typically programs offer video interviews to applicants they are considering. Three rounds of offers are made — the first two at noon and 3 p.m. Wednesday, and the third (final) round at 9 a.m. Thursday. If you receive an offer, you have 2 hours to accept or reject. It is against NRMP rules for you (or any advisors acting on your behalf) to contact program directors of unfilled spots until the program has contacted you first.
Once the SOAP rounds are completed, all remaining open spots will be listed. At that point, students can contact programs directly.
Military Match: Military spots available will be published on MODS.
What are my options?
Realistically, matching into EM via SOAP is extremely unlikely, although if any EM spots are open you should pursue them. In 2017, 99.7% of the 2,047 spots filled; this left 6 spots open. In 2016, there was 1 spot open.1 If you have not matched, the real decision you need to make is whether to try to obtain a one-year position and then reapply to EM, choose another specialty, or do a non-clinical year.
Occasionally there may be a new residency in EM that receives approval after the NRMP process, and students who have not matched at first or through SOAP are eligible to contact those sites directly. An EM advisor actively involved in the application process should know if they exist and can direct you to them.
If you decide to do a preliminary year of post-graduate training in another specialty, make sure you go to an academic institution with an emergency medicine residency program. Secure an early rotation in the ED so those folks can advocate for you and write a letter. Be open and honest with the program leadership about your situation and you’ll find many people willing to help guide you to success. A 2018 survey of program leaders showed most believe the best use of time is to SOAP into a prelim year and reapply the following year.4 Further, they preferred the applicant perform the prelim year in a surgical or medicine department. There are a few new options for EM/Critical Care preliminary years, which include extensive training in both EM and critical care. They have the advantage of continued exposure and training directly applicable to EM and a letter of recommendation from an EM clinician, familiar with EM training.
Table 12.1 Gap Year Options
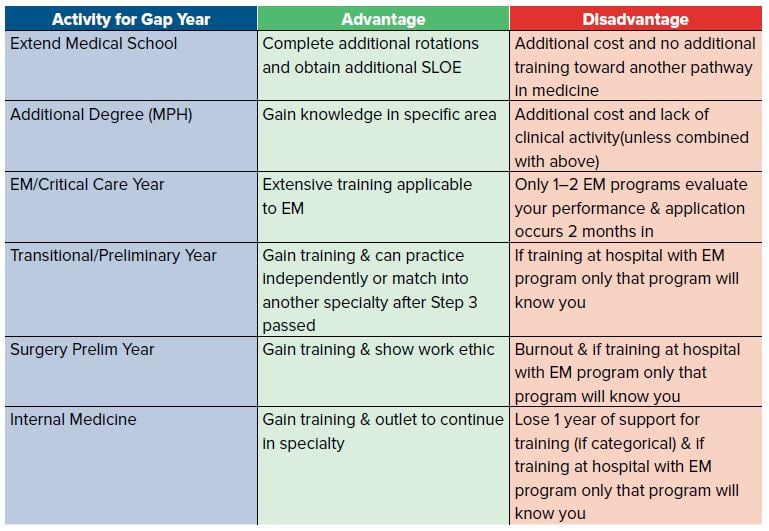
Non-clinical choices include obtaining an MPH, performing a research year, extending medical school to a 5th year, or obtaining some other type of graduate degree. These are all reasonable options, but be ready to explain how this better prepared you when you re-apply to EM. Choosing one of these paths does give you the opportunity to apply for positions that become available after the match (assuming you have not chosen an option with a binding contract). If you choose to do research, do so with an emergency physician. If you choose another non-clinical route, find ways to stay involved with the EM program in your facility. You can also consider rotating in EM in the months just prior to graduation to get an additional SLOE.
In the past, applicants have decided on a different specialty, such as internal medicine or family medicine, and then worked in the ED after graduation. These positions were often available in more rural areas, but are becoming rare. This is not an effective pathway to the independent practice of emergency medicine and is not recommended.
Military Match: Military applicants who do not match typically enter a transitional year or a GMO (general medical officer) assignment. In general, it is harder to match into EM out of a transitional year than a GMO assignment after not matching.
Re-application
Re-applying for residency is a red flag for many programs. The fact you are reapplying cannot be hidden, and you have very little time before the next application cycle begins. Be honest about your deficiencies, and address the ones that are possible to alter. You cannot change your Step 1 or 2 scores. You cannot change your transcript or felonies. You can, however, prove your work ethic, add a stronger SLOE, show your dedication to the field, and make more contacts through conferences, social media, presenting research, etc.
If you think a SLOE from your previous year may have prevented you from matching, choose which letters to re-submit with your new application. Even if you do ask that a SLOE be re-submitted, sit down with the letter writer, try to show what you have done to improve yourself, and ask them to revise the SLOE accordingly. Consider completing additional EM rotations before you graduate in order to obtain new SLOEs that are more supportive. While it will be clear what you have done, if these new SLOE are supportive they will help your application more than a less supportive original SLOE.
If your interview skills are not strong, practice. Find friends and advisors to give you frank commentary on those skills.
The LoR from your program director if you are in a clinical year (eg, preliminary surgery or medicine) can address changes in your abilities and work ethic. It is important to note that you will have only worked with them for a couple of months by this point, so their LoR may not be as influential as the EM program directors’ letters.
If you are in a categorical residency, you need your PD’s permission and LoR for re-application. Also, if you match into a categorical residency position outside of EM and then decide to re-apply, some places will not be able to interview you because of funding issues. The government assigns funding based on your first categorical match in a particular specialty for a certain number of years — which can often create a shortfall because of the difference in lengths of residencies. Prelim years do not count. If you initially match into a 4- or 5-year categorical in a different specialty and are re-applying, the government will provide funding for the number of categorical years you would have had remaining.
If you decide to re-apply, you need to understand your chances are certainly not universally better. You may improve your chances at a few places that now know you better, or are willing to meet you, but statistically, your chances of matching into EM are diminished. In the 2018 NRMP program director survey approximately one-quarter of program directors indicated they often interview or rank prior graduates, and approximately two-thirds responded they seldom do.5 Even interviewing itself is more challenging if you are in a clinical year and need to find creative ways to get time off to travel. You may be limited on how many times you can leave for interviews per month. A back-up plan is even more crucial, because a second re-application to EM is even less likely to be successful.
The Bottom Line
- The most important step to take if you don’t match is to find an advisor well-versed in EM application/re-application. Sit and talk through your application to identify what likely contributed to you not matching, and to construct a personalized strategy to move forward.
- The SOAP allows you to apply for open spots within EM for this match, if any are available. You can also choose to apply in another specialty or for a preliminary position during SOAP.
- There are multiple approaches to re-application in EM, including extending medical school, pursuing a year of training and completing an additional degree or experience. Each of these has advantages and disadvantages for re-application in EM.




