Guide to the History and Physical
Presenting to an ED can be anxiety-provoking for all patients, but especially so for trans patients. It is critically important to create a safe, sensitive, and trusting environment by employing specific questions, terminology, and physical exam techniques.
The first rule: Do not make assumptions! Specifically, do not assume a patient's gender, sex, or sexual orientation until clarifying with the patient.
This chapter will review how to establish a rapport with trans patients, and provide specific history-related questions and terminology to use when asking these sensitive questions. An overview of physical exam approach and techniques will also be reviewed, with specific regard to patients undergoing hormone therapy and in the setting of gender-affirmation surgery.
History
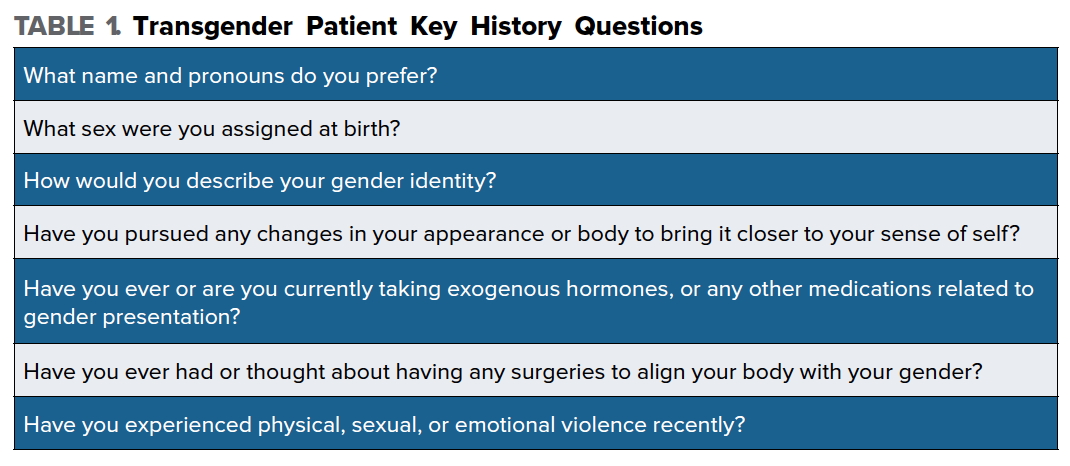
Name + Pronouns
Start by establishing by what name and pronouns the patient would like to use, as this may differ from what is recorded in the chart. Simply ask, "What name and pronouns do you prefer?" Getting this right is the single most important thing you can do to put trans patients at ease. If you make a mistake with language, be sure to apologize prior to moving on. Patients will appreciate your recognition of the error.
Sex + Gender
Explore the patient's sex and gender identity, as these are two distinct entities for the transgender patient. Sex refers to the biological and physiological characteristics that define men and women, while gender refers to socially constructed roles, behaviors, activities, and attributes society considers appropriate for men vs. women. Keeping questions open-ended is extremely important, as it gives the patient an opportunity to describe themselves in their own words. For example, ask "What sex were you assigned at birth?" or "How would you describe your gender identity?"
Hormone Therapy + Gender Affirmation Surgery
Not all trans patients will be taking exogenous hormones or will have undergone surgical approaches to alter their physical appearance. Thus, it is important to obtain this history from every trans patient in order to provide appropriate care. An easy initial question to broach this topic is, "Have you pursued any changes in your appearance or body to bring it closer to your sense of self?" If the answer does not elicit specific information about hormone and surgical history, then probe further. Ask "Have you ever or are you currently taking exogenous hormones or any other medications related to gender presentation?" If the answer is yes, be sure to ask where they are getting these hormones, as some patients may be taking unregulated hormones they buy online without the guidance of a physician.
With regard to surgical history ask, "Have you ever had or thought about having any surgeries to align your body with your gender?" Knowing if your patient has had surgery, and what kind, will help guide the physical exam.
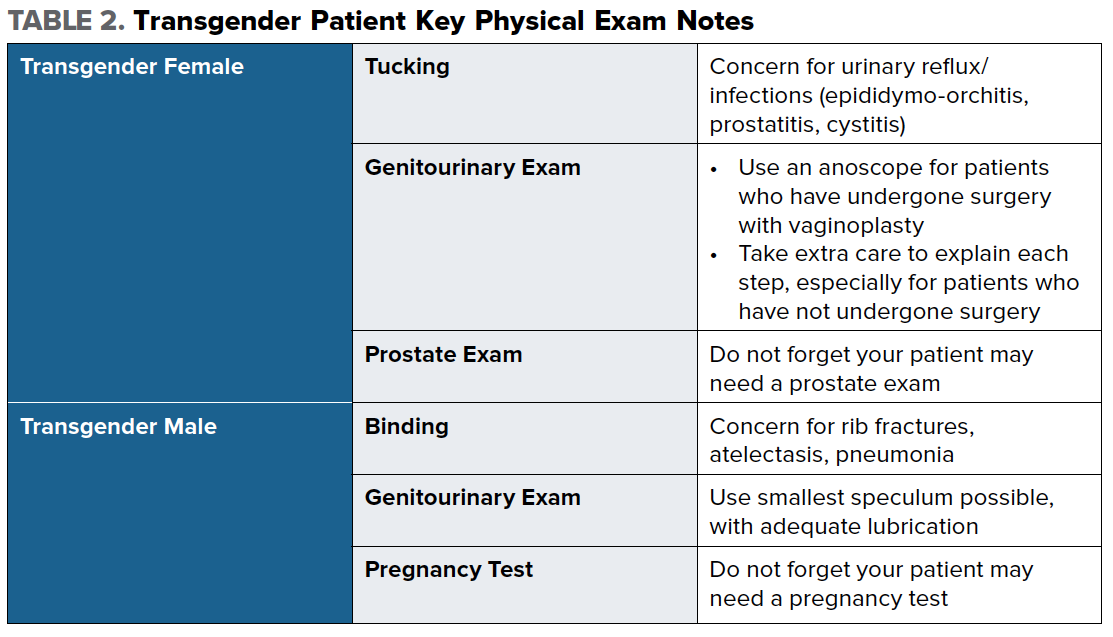
It is also important to ask patients about tucking, which may be done by transgender female patients who have not undergone gender affirming surgery. It is performed by manually displacing the testes upward into the inguinal canal, and then positioning the penis and scrotal skin between the legs and rearward. Applying tight underwear, tape, or a gaff (special garment) helps to maintain this positioning. Prolonged periods of tucking, which places the urethral meatus close to the anus, may result in urinary reflux or infection, such as epididymo-orchitis, prostatitis, or cystitis.
Some trans men who have not undergone top surgery may bind their chests, and if this is done too tightly or for an extended period of time, it can put these patients at risk for rib fractures, atelectasis, or even pneumonia.
Sexual History
Transgender patients have higher rates of engagement in sex work and HIV infection. Because of this, every physician must take a detailed sexual history in order to tailor their care appropriately.
Start with the familiar, "Are you currently sexually active?" but also obtain specific information as to what kind of sex (oral, anal, and/or vaginal) and with whom (men, women, both, other). For example, a transgender male may still have female reproductive organs, and if they've had vaginal receptive intercourse with a cisgender man, they need to be screened for pregnancy. They are also still at risk for diseases such as ovarian torsion and pelvic inflammatory disease. Additionally, this patient may need referral to a gynecologist for regular check-ups, including pap smears.
It is important to approach these questions with particular detail to language, and ask patients what kind of language they use to refer to their body. For instance, some patients may be uncomfortable with the term "vagina" and may use another term instead. In addition, a transgender female may have male reproductive organs and is at risk for diseases such as prostatitis, prostate cancer, and testicular torsion. In general when taking a sexual history, it is always a good idea to ask about the pelvic organs your patient has, as well as those of their partners, and once again try not to make assumptions.
Social History
Transgender patients are at a higher risk for intimate partner violence, suicide, illicit drug and alcohol use, and homelessness, when compared to the general population. Screening for these entities is a key part of the history, and referral to social work is important so patients know what resources are available to them.
Approaching the topic of violence can be uncomfortable, but it cannot be avoided. Initiate the conversation by asking, "Have you experienced physical, sexual, or emotional violence recently?"
All patients should be screened for depression and possible suicidality. Providers can use the Patient Health Questionnaire-2 (PHQ-2) to screen for depression. Ask, "How has your mood been? Have you been feeling depressed or hopeless? Have you ever thought you would be better off dead? Have you thought about hurting yourself in any way?"
Homelessness is a complex issue for transgender patients - not only because they exhibit high rates of homelessness, but also because finding a safe shelter can be very difficult. Based on where you practice, there may be specific resources and shelter for trans patients, and social workers can help with information and referral.
With regard to questioning about illicit drug and alcohol use, approach this is in a similar manner as you do with all patients.
Physical Exam
This section will provide special considerations to make your trans patients feel more comfortable during the physical exam. First and foremost, do not perform any unnecessary physical exam maneuvers that are not relevant to the patient’s chief complaint or invite unnecessary team members into the room, as many trans patients have described feeling like a “specimen” or “spectacle” on display. If you must examine a sensitive area, be sure to ask permission and also explain why it would impact their medical care, as you would with any patient.
Transgender Male
The pelvic exam may be a traumatic and anxiety-inducing procedure for trans men, especially if they have not undergone gender affirming surgery. Again, you can start by asking a patient how they refer to their anatomy and if they are comfortable using words like vagina to describe their anatomy. If a patient has not had gender affirming surgery and thus still has female reproductive organs, but is taking exogenous testosterone, this can induce a hypo-estrogen state, which promotes atrophy, increases vaginal pH, and increases the risk of vaginitis and cervicitis. In order to perform a pelvic exam, it is advisable to use the smallest speculum available, or even an anoscope, to reduce pain and trauma. Give the patient an overview of how you will perform the exam, and alert them of each step before you do it.
Transgender Female
Whether or not a transgender female patient has undergone gender affirming surgery will dictate how you perform the physical exam. For patients who have undergone surgery with vaginoplasty, the recommendation is to use an anoscope for the pelvic exam. After inserting the anoscope, the trocar is removed, and the walls of the neo-vagina can be visualized.
For patients who have not undergone gender affirming surgery, approach the genitourinary exam with sensitivity by explaining everything before it is performed, and pay particular attention to whether a patient practices prolonged tucking. When appropriate, based on the patient’s chief complaint, do not forget that these patients, regardless of surgical history, likely still have a prostate and may need a prostate exam.