Ch. 6 - Crush Your Clerkships, Secure Your SLOEs
Three years of hard work have flown by, and you have earned the opportunity to explore EM and demonstrate your skills during your EM clerkships. Two of the most important factors of your application, your clerkship grades and your eSLOE, are a result of your rotation performance. These factors carry significant weight in how most programs determine interview invitations and rank order list positions. You’re about to begin your EM rotation, and you have one burning question:
What can I do to stand out and make a positive impression during my clerkship?
First, remember some basic practices that may seem small but in reality will be the foundation of your performance.
- Be on time. Even better, be early. Showing up late to a shift or didactic session is unprofessional and demonstrates a lack of enthusiasm. If you need to miss a day or will be late, notify your clerkship director as soon as possible. During an away rotation, take into account the commute time from your housing to your clinical site before your first day.
- Dress appropriately. Ask how you are expected to dress (scrubs, business casual, white coat, etc.) on shift, during conferences, and in didactic sessions.
- Be (appropriately) enthusiastic. Your enthusiasm for learning will be noticed quickly and much appreciated. It will also help you get the most out of your rotation.
- Come prepared. Make sure to bring your stethoscope, trauma shears, and a pen (or two!) to every shift. Also, consider having handy pocket EM guides or medical apps on your phone for quick references on shift. We’ve included some suggestions later in this chapter.
Next, remember that you are an important member of the team. Your evaluations and plans matter, even if at times you feel they don’t. Along with the nursing staff, you will often be the first person to meet patients. You will also usually be the person spending the longest time with the patient. Therefore, your history and physical will be instrumental in creating the plan moving forward.
IMG Candidates: Non-native English speakers will need to demonstrate mastery of the English language to show they can communicate well, both with patients and other members of the care team.
Preparing for a Successful Clerkship
It’s important to build your fund of EM-specific knowledge. This occurs before, during, and after clinical rotations. Take advantage of the many resources available to you — as you prepare for, during, and after you crush your clerkships.
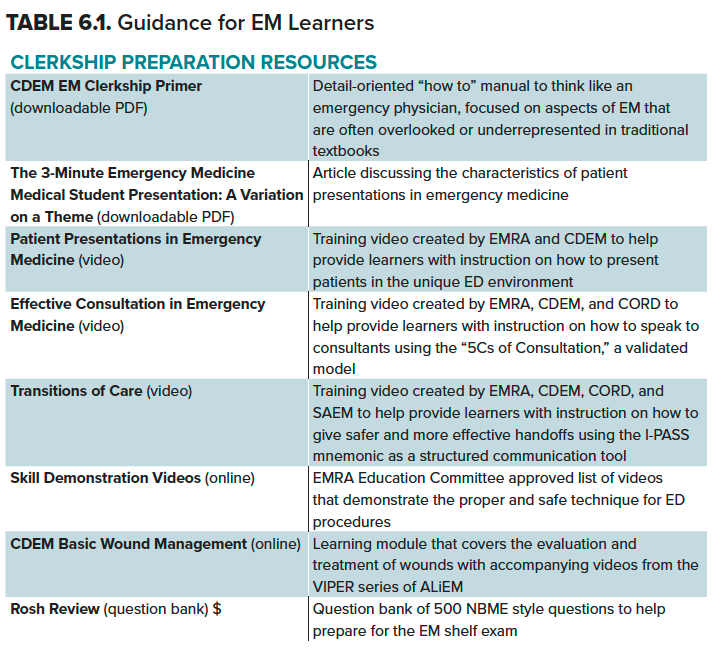
You might feel like there’s an overwhelming number of resources; test several of them before your clerkship and use the ones you feel most comfortable with.
Interacting with Patients
While you’re brushing up on the clinical aspects of patient care, don’t forget the patient. It’s important to establish rapport quickly, but that can be challenging when you’re approaching a stranger who’s experiencing a problem grave enough to lead them to the ED. Follow some basic steps:
- Introduce yourself to the patient, and explain your role as a medical student.
- Find out who is accompanying them (do not make assumptions).
- Ask why they’re in the ED today. For chronic conditions, find out what made today different than any other day, and research prior treatments.
- Determine if they’ve had any prior work-up relevant to today’s visit and where these records can be located.
- Inquire about their access to follow-up care.
- Small things go a long way with patients and their visitors: Does the patient need a blanket? A phone to call their loved one? Does their elderly visitor need a chair?
- If your initial impression is the patient is unstable, agitated, or altered, you are probably right, and in such instances, get your resident or attending immediately to evaluate the patient.
Presenting a Patient
Your oral presentation to your attending is critical in demonstrating your knowledge of a patient’s complaint, exam, and management plan. But a patient presentation in EM is unique. The pace of the ED environment demands extremely succinct presentations that may be interrupted at any given time — be thorough yet brief, and be ready to pick up where you left off after any interruptions. Focus your presentation to include the patient’s chief complaint and any information relevant (positive or negative) to the complaint, also noting relevant exam findings. Then, present your differential diagnosis, prioritizing the most emergent diagnoses, and discuss your anticipated management plan. While presenting your plan, consider including any consultations you might need and anticipated final disposition if it is apparent. Be ready to answer any additional questions about the history and physical exam, but this does NOT mean you need to present every detail initially; stick to what you know is relevant to the chief complaint.
Developing a Strong DDx and Plan
Your differential diagnosis should be based on your history and physical exam. Do not rattle off a random assortment of diagnoses, as this reflects poorly on your medical decision-making. Do include all emergent diagnoses in your differential, even those that are less likely or don’t require further work-up, to demonstrate to your evaluator that you’ve considered all possibilities. A good framework to organize your differential is SPIT:1
- Serious
- Probable
- Interesting
- Treatable
Utilize your differential to decide which labs, imaging, and interventions are needed. Familiarize yourself with the clinical prediction rules your supervising resident or attending will consider when determining what work-up is necessary, such as the HEART Score for ACS, the Wells’ and PERC scores for PE, the Canadian CT Head rule for trauma, etc. Of note, MDCalc is a great central location to find all these decision-making tools!
Be ready to discuss your anticipated disposition for the patient, including what type of follow-up they might need. If you don’t verbalize your thinking, your supervisor won’t know what you’ve considered and won’t be able to give you meaningful feedback on your presentations. Expect to be quizzed after you present your differential and plan. These questions are not casting doubt on your competence, but rather they enable your evaluator to understand your thought process and provide an opportunity to strengthen or modify your plan.
NEVER LIE. If you didn’t ask a question about a patient’s history, forgot to check for something during your physical exam, or didn’t consider a specific diagnosis when generating your differential, absolutely do not lie! It takes time to gain the trust of your supervisor, but that trust can evaporate quickly. When you are open and honest about what you did or didn’t do, it assures that the rest of your presentation is honest and accurate. You can always go back into a patient’s room to collect the missing information. But if there is even a hint that your presentation was not honest, it creates more work for your supervisors because they must start with a blank slate.
DON'T OVERREACH. There’s a first time for every procedure — when that’s the case, simply let your supervising physician know you’ve never performed the procedure, but you would like to learn and practice. Similarly, if you are asked a question you cannot answer, say you don’t know, and then go find an answer. Admitting you don’t know something doesn’t show incompetence, it demonstrates humility — patients and attendings alike will respect this.
"OWN" YOUR PATIENTS. Depending on your rotation and electronic chart access, this can be difficult. In general, you should stay on top of lab/imaging results and recognize their relative impact on care. For example, if a urinalysis comes back suggesting UTI, reporting this to the resident/attending and suggesting an appropriate antibiotic choice and disposition would be excellent care. Remember — anyone can report abnormal findings, but the real question is what to do with those findings.
Ownership also includes updating patients with plans and results and managing their expectations for their visit. This is easier for you as a student, simply because you’ll have more time than your resident/attending. Show ownership by reassessing after interventions (eg, the nauseous patient no longer vomiting after receiving antiemetics) and re-evaluating physical exams as needed (eg, serial abdominal exams). Furthermore, inform your attending of any status updates with your patients, reassessments, or results. You are often the best eyes and ears for your attending. Recognizing a critical change or “sick” patient and immediately alerting the ED team of this will always garner respect.
If given tasks to complete (notes, consults, procedures) do them promptly and inform your supervising resident or attending when you’re finished. If you encounter difficulty, that’s okay — just let the team know. If you have completed all tasks for a patient, you can demonstrate initiative by asking to pick up another patient. However, be sure not to pick up so many that you fall behind. You will impress your attending far more by providing thorough, complete care to fewer patients than by superficially involving yourself with a lot of patients.
GROW. As you become more comfortable in the ED, challenge yourself to pick up one more patient than your prior shift, still being sure not to get overloaded. Set an alarm or timer for your history and physical exams to practice becoming more efficient, without cutting corners. For patients undergoing procedures, familiarize yourself with the steps of the process and the supplies needed, and express an interest in performing or assisting whenever possible.
TALK TO YOUR TEAM. Check in with your supervisor at the start of every shift. Introduce yourself and identify their expectations and responsibilities. These may change from attending to attending, shift to shift, and it’s important to recognize these differences. Examples of these are:
- Should you assign yourself to the next patient or should you ask permission before assigning yourself to new patients?
- Should you present before or after writing your note?
- Are you responsible for writing your own orders?
Clear communication at the beginning of each shift also enables you to show that you are engaged with specific goals. For example, “Today my specific goal is to work on X, and I’d love feedback on it.” At the end of the shift follow up on this goal and seek constructive criticism.
Lastly, communicate with the entire team (attendings, residents, nurses, consultants, health unit coordinator, techs, etc.) respectfully and pleasantly. Learn their names. Let them know you are there and eager to be a part of patient care. This allows them to show you interesting cases, teach you procedures, and include you throughout the course of your shift.
ASK QUESTIONS. If you are unsure about something, ask! Asking questions reflects an interest in learning and demonstrates you are thinking about your patient’s presentation. Remember, we know you’re a medical student and you’re here to learn. It’s our responsibility to educate medical students, and most teaching departments work to foster learning. Of course, there is a balance — before asking a question, consider looking up the answer to your question and be ready to discuss possible management strategies. A good way to phrase this (and demonstrate self-motivation) is, “I have a question regarding the management of X. I’ve read that we can do Y, however, I was wondering if that’s the appropriate course in the setting of...” Also, make sure to “read the room” before asking a question. Unless your question involves an emergent issue, certain times in the ED may not be appropriate for discussions and feedback (eg, during sign-out, while the team is taking care of a critically ill patient, etc.).
If you are unsure about something (how to call a consult, discharge a patient, etc.), ask your attending or team members. In general, we recommend asking residents first, as sometimes the attending is managing multiple other tasks.
ACE THE FINAL EXAM. Depending on your rotation site, you may take an exam created by that department or by a national organization. Be sure to inquire about what resources are recommended for preparation (readings, practice questions, etc.). Free and fee-based question banks are widely available. Do some reading, flashcards, and practice questions each day to build your knowledge base and prepare for the exam.
ATTEND CONFERENCE. Many sites integrate this into your clerkship schedule. However, if not, ask if you can attend weekly resident conferences. Your interest will be noticed, and it will allow you to see what’s new in EM, get to know more of the residents, and see what your weekly educational experience would look like if you match at that program.
BE KIND. Think of your clerkship as a month-long interview, remembering that your interactions with everyone, from attendings and residents to ED staff to the residency coordinator, will be noted. Be unfailingly kind, courteous, and professional.
LOOK AHEAD. Clerkships are the perfect chance to build your professional network by meeting attendings, residents, and administrators and connecting with other students who are rotating with you — because they could be one of your fellow residents next year. Along the same lines, get to know the city where you’re rotating; can you see yourself living there? Finally, find out upfront whether an interview will be offered at the end of your clerkship — this data is also available in EMRA Clerkship Match.
Remember that while you’re continually being graded during your clerkship, this is also your opportunity to evaluate the program. Do you like the atmosphere, the residents, the attendings, and the opportunities? These rotations will be the basis for how you evaluate each program where you interview.
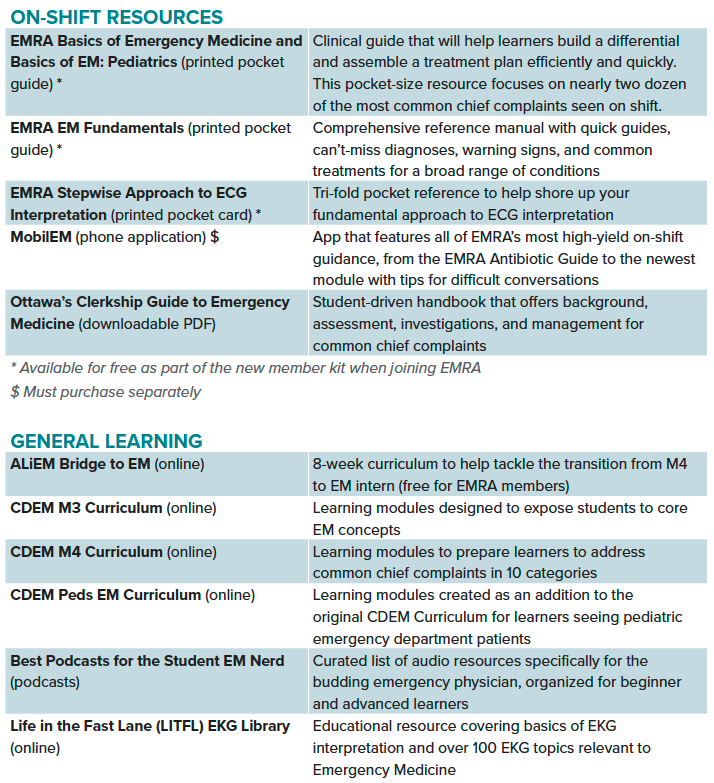
Demystifying the SLOE
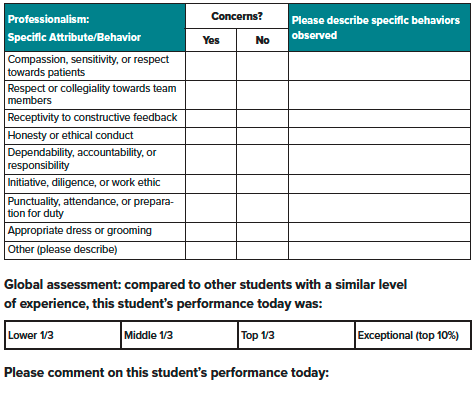
Now, let’s look at the criteria you will be evaluated on from that dreaded (mysterious?) eSLOE. Why is this important? Program directors have ranked eSLOEs (and rotation grades) as some of the most important criteria when looking at selecting potential residents.2 Therefore, understanding the eSLOE provides insight into how you will be formally evaluated. In 2022, the eSLOE was updated — see figure 6.2 for an example of the updated eSLOE. Review the eSLOE form before your EM rotation to understand the characteristics by which you will be judged.
The updated eSLOE has seven sections: In the “Demographic Data” and “Background Information” sections, programs outline the sources of information they used in compiling the eSLOE and the primary letter authors’ nature of contact with the applicant — see figure 6.2 to see all the possible options in these sections. These first sections also include information on when the applicant rotated with the program, what grade was given, how the student’s grade compares to others in the prior academic year, and if there was an exam taken during the rotation how the applicant’s grade compares to their peers.
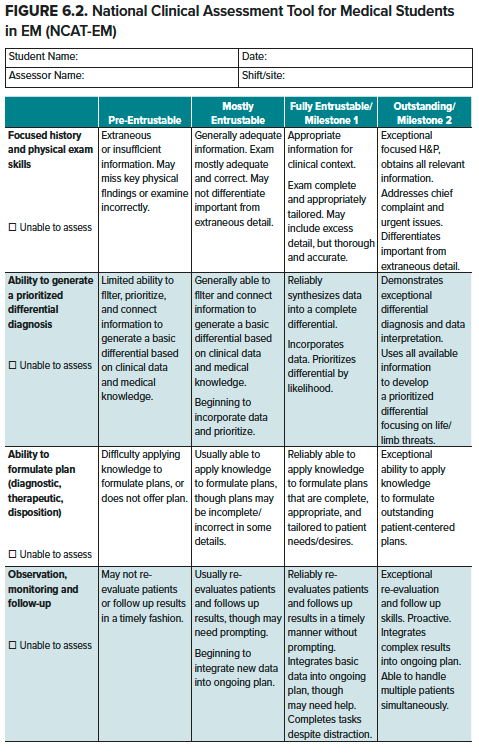
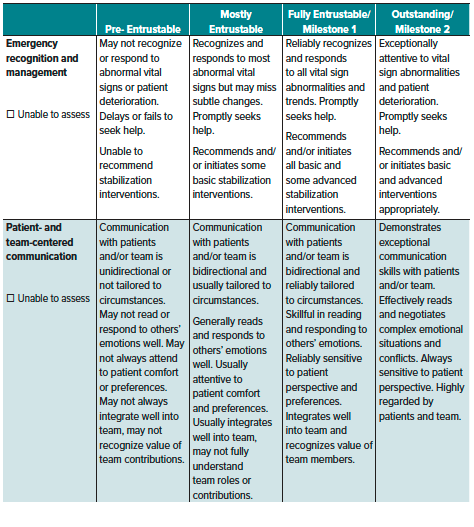
“Evaluation of Student: Part A” is a competency-based evaluation, which means students are NOT compared to their peers. “Part A” is based upon the National Clinical Assessment Tool for Medical Students in EM domains — see figure 6.3 for an example of the NCAT-EM, with entrustability anchor descriptions. Students are evaluated on their entrustability in the following areas:
- Ability to perform a focused history and physical exam
- Ability to generate a differential diagnosis
- Ability to formulate a plan
- Ability to perform common ED procedures
- Ability to recognize and manage basic emergent situations
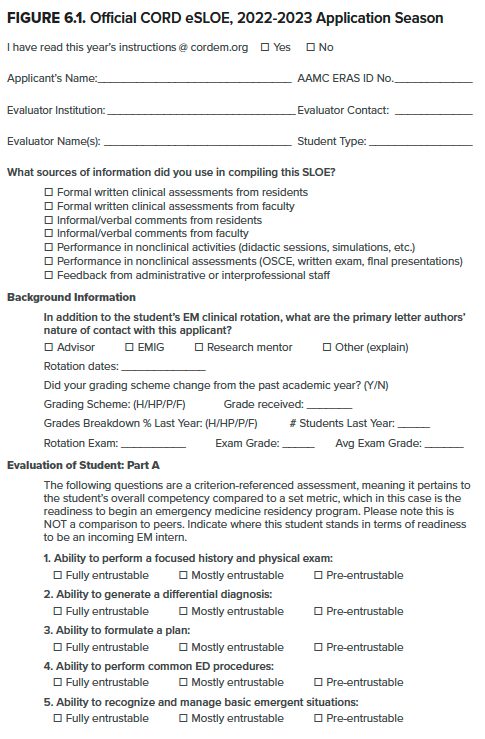
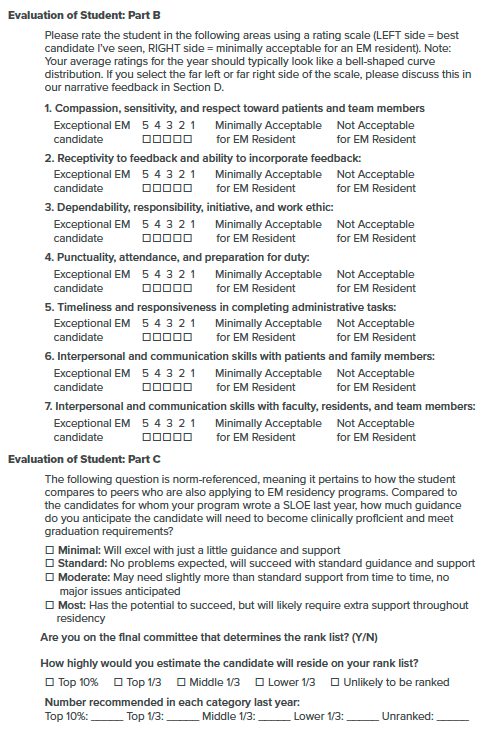
“Evaluation of Student: Part B” is norm-referenced (how the student compares to his/her/their peers who are also applying to EM), using a 1-5 rating scale (with 5 being the best and 1 being minimally acceptable for an EM resident), in the following areas:
- Compassion, sensitivity, and respect towards patients and team members
- Receptivity to feedback and ability to incorporate feedback
- Dependability, responsibility, initiative, and work ethic
- Punctuality, attendance, and preparation for duty
- Timeliness and responsiveness in completing administrative tasks
- Interpersonal and communication skills with patients and family members
- Interpersonal and communication skills with faculty, residents, and health care professionals
“Evaluation of Student: Part C” is also norm-referenced and asks how much guidance programs anticipate the student will require to become clinically proficient and meet EM residency graduation requirements. The following are options:
- Minimal: Will excel with just a little guidance and support.
- Standard: No problems expected, will succeed with standard guidance and support.
- Moderate: May need slightly more than the standard support from time to time, no major issues anticipated.
- Most: Has the potential to succeed, but will likely require extra support throughout residency.
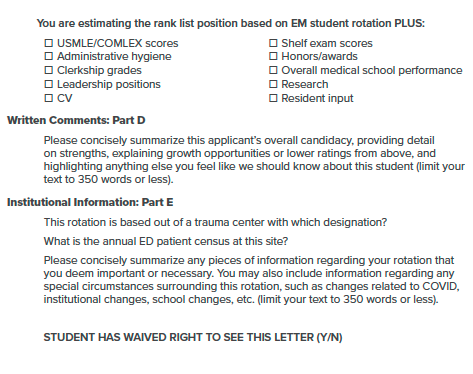
In this section, we anticipate the majority of students should fall into the standard guidance category. While you cannot see your eSLOE, if feedback from your rotations and/or your final clerkship grades indicate you might fall into moderate or most guidance categories, you should reach out to your EMspecific advisor for guidance. “Evaluation of Student: Part C” also asks how highly the program estimates the student will reside on their rank list: Top 10%, Top ⅓, Middle ⅓, Lower ⅓, or Unlikely to be on their rank list. Programs can select what criteria they are basing this rank list position on — see figure 6.2 to see all the possible options programs can select. As a reminder, before late September when ERAS opens to programs for review, programs do not have access to your entire ERAS application at the time they submit your eSLOE. Thus, there are other items (such as eSLOEs from other programs, your Dean’s Letter/Medical Student Performance Evaluation, Step 2 score, etc.) that might affect your rank list position, and this is an estimation of the rank list position at the time the eSLOE is written and submitted — it is always subject to change later in the application/ interview season.
The “Written Comments: Part D” section asks programs to summarize the student’s overall candidacy, providing detail on strengths, explaining growth opportunities or lower ratings from the other sections, and highlighting anything else they feel other programs should know about the student.
Finally, “Institutional Information: Part E” allows the program to put information about their trauma center designation, annual ED patient census, and any other pieces of information regarding their rotation that they deem important or necessary for other programs to know about. At the end of the day, the eSLOE provides other programs insight into your perceived professional/personal strengths and areas that might need focused attention during residency, and it enables writers to highlight both as they feel necessary.
Whom do I ask for my SLOE?
Most programs have a plan in place for rotators to obtain an eSLOE. Some rotations will say who will handle the eSLOE at the clerkship orientation, whereas others will have students formally ask. Typically you will ask the clerkship director to complete your eSLOE. However, some clerkships will ask you to obtain an eSLOE from the faculty who knows you best. If this is the case, try to identify a faculty member early on in the rotation. Many academic departments complete a “departmental eSLOE” — a jointly signed letter from the clerkship director, program director, and associate program directors, which carries more weight than an eSLOE written and signed by a single faculty member.
Clarify the process by which you will obtain your eSLOE on the first day of your rotation.3 Importantly, it is expected that you will have an eSLOE from each site at which you rotated. Not having an eSLOE will be perceived as a red flag and may require an explanation if you are invited for an interview. An exception to this is rotations that are scheduled later in the application cycle. If you have already submitted two eSLOEs and you are completing a third EM rotation later in the year (eg, December), you do not necessarily need to obtain an eSLOE from this rotation.
End-of-Shift Feedback/Evaluations
While the eSLOE is a summary evaluation of your performance for your entire rotation, it is crafted based on the cumulative feedback/evaluations you receive for each shift. Students should determine who will be evaluating them at the end of each shift — will it be an attending, a senior resident, or both?
While you are being evaluated and graded continually by the faculty and upper-level residents during your clerkship, you should not be a passive bystander. Seek feedback early and often — even if that means waiting for your supervising resident or attending to finish signing out (while being respectful of their time). Be prepared to explain what you think you did well, what you would do differently, and how you plan to improve on the next shift.
In addition to familiarizing yourself with the contents of the eSLOE, you should also familiarize yourself with the end-of-shift evaluation tool that will be used to judge your performance. Many clerkships have adopted the NCAT-EM to provide standardized evaluation across institutions, calculating a final grade by averaging NCAT-EM scores from at least six shifts. The NCAT-EM evaluates a student’s performance in six clinical performance domains, along with an assessment of the student’s professionalism during a shift (see figure 6.2).4
The Bottom Line
- Performing well on your EM rotation requires knowing the differential diagnoses for common chief complaints, being able to synthesize and succinctly present patients to your attending or supervising resident (including your plan), “owning” and re-evaluating your patients, and being a great team player and communicator.
- Ask for feedback! Familiarize yourself with the tools that will be used in your evaluation so you can focus on demonstrating behaviors that will give you a competitive eSLOE.
- Make use of resources, such as the Patient Presentations in Emergency Medicine instructional video, to learn how to effectively and efficiently tell your patient’s story.
- Do not under any circumstances lie about the patient history you take or an exam finding. Your supervisors know you’re learning, and they don’t expect perfection. They do expect honesty — and it will take a long time, if ever, to earn back trust if you lie.
References
- Chinai SA, Guth T, Lovell E, Epter M. Taking Advantage of the Teachable Moment: A Review of Learner-Centered Clinical Teaching Models. West J Emerg Med. 2018;19(1):28-34.
- Negaard M, Assimacopoulos E, Harland K, Van Heukelom J. Emergency Medicine Residency Selection Criteria: An Update and Comparison. AEM Educ Train. 2018;2(2):146-153.
- Lutfy-Clayton L, Morrissey T, Pelletier-Bui A, et al. The Emergency Medicine Applying Guide. Council of Emergency Medicine Residency Directors Advising Students Committee in Emergency Medicine. 2018.
- Jung J, Franzen D, Lawson L, et al. The National Clinical Assessment Tool for Medical Students in the Emergency Department (NCAT-EM). West J Emerg Med. 2018;19(1):66-74.