Ch. 7 - Building Your ResidencyCAS Application
Updated 2025 by:
FACULTY
Alexis Pelletier-Bui, MD | Cooper Medical School of Rowan University/Cooper University Hospital
Elizabeth Barrall Werley, MD | Penn State Health Hershey Medical Center/Penn State College of Medicine
Tim Fallon, MD | Maine Health Maine Medical Center Portland, Tufts University School of Medicine
Erin McDonough, MD | University of Cincinnati College of Medicine
Liza Smith, MD | University of Massachusetts Chan School of Medicine - Baystate
STUDENT REVIEWERS
Zoee Castro, BS, MSIV | University of Nevada, Reno SOM
Chair - 2025 EMRA Medical Student Council
Atira Shenoy, BS, OMS-III | Nova Southeastern University
Vice Chair - 2025 EMRA Medical Student Council
Kiersten Diercks, BA, MSIII | UT Southwestern Medical Center
Student Advising Coordinator - 2025 EMRA Medical Student Council
EDITOR-IN-CHIEF
Erin Karl, MD, MEHP |Hennepin County Medical Center
By now, you have started to consider the different types of EM residency programs available (Chapter 4), you have completed or scheduled your EM clerkships and USMLE/COMLEX exams (Chapters 3 and 5), and it's time to understand how you actually go about applying to residency programs.
The application has several components, and each will impact your competitiveness (Chapter 8). Be sure to connect with your advisor as you build your application to discuss your unique concerns and help guide your decision-making. As a reminder, students at schools without an EM residency or EM advising can email distanceadvising@cordjobboard.com for help finding an advisor.
ResidencyCAS
ResidencyCAS is a centralized application service offered by Liaison International.1 This platform has been in use in health care and other settings for decades, and it was first used in the world of graduate medical education (GME) by OB/GYN programs in the 2024-2025 residency application cycle. Emergency medicine programs will be utilizing ResidencyCAS for the 2025-2026 application cycle.2 Your ResidencyCAS application will provide a great deal of information about you, and residency leaders will use it to consider you for an interview invitation, to help prompt interview discussion, and to determine your position on their rank list.
At the time of publication of this guide, EMRA and CORD anticipate that all EM residency programs will transition to ResidencyCAS for the 2025-2026 season. You can refer to the CORD Emergency Medicine Collaboration with ResidencyCAS page for more updates.
How Do I Create a ResidencyCAS Account?
Registering for ResidencyCAS requires an individual access link that will be provided to you by your medical school’s Dean’s office.3
IMG Candidates: Visit ECFMG.org to fill out a "Residency Application Support Form" and pay an associated fee. Once the form is received and processed, a member of ECFMG's residency application support team will contact you with specific information and instructions for document submission. Your instructions might vary depending on several factors, such as whether you are participating in multiple residency application services. Further access information will be provided by ECFMG. Graduates of Canadian medical schools should visit CaRMS.ca for information on how to register for ResidencyCAS. To receive access to the ResidencyCAS application portal, send an email to eras@carms.ca with the following information: First name, last name, medical school, and your email. The email address you provide must match the one you will use when completing your residency application.
Military Match: The military uses a separate application system through MODS (Medical Operational Data System). However, you must also apply through ResidencyCAS to be considered for civilian programs in case of deferment.
Know The Timeline
Keep key dates in mind when approaching the application process, and mark them on your calendar. The first is the date when ResidencyCAS opens and you can begin editing your application and uploading documents, typically in early June to allow you ample time to work through the steps of your application, request letters, and determine which programs you will be applying to/signaling before the start of the season.
Applications will be due in late September, and it is important to have your application submitted by this deadline. Exact dates may vary between cycles – double check the ResidencyCAS website for your year, and mark these dates on your calendar!
Residency programs are granted access to applications and supporting documents on a set date after the submission deadline, typically in late September/early October.
Stick to the Timeline!
You must submit your application before residency programs are granted access. In a prior survey of PDs, only 15% of respondents stated that it was "highly likely" that an application would be reviewed if it were completed after applications become available to residency programs.4
Regardless of when you apply, once you certify and submit your application, you will not be able to make changes other than editing your contact information, adding new entries to certain areas of the "Supporting Information" and "Program Materials" sections, adding additional programs, or uploading additional letters of recommendation.
Military Match: The deadline for initial application to military programs through MODS is the second week of September, and supporting documents are typically due mid-October. Rank lists are usually submitted around this time as well. Keep these military-specific deadlines in mind as you must complete both MODS and ResidencyCAS simultaneously.
Latecomers: Do not wait for rotations or letters to submit your application. Submit it on time, and update it with additional documents as they become available. A program will wait for a letter, but if your application isn't in by the deadline, they are unlikely to seriously consider you.4
The Components of ResidencyCAS
- Personal information
- Biographic information
- Contact information
- Geographic connections
- Race & ethnicity
- Work authorization
- Other information
- Language proficiency
- Pell Grant recipient
- First-generation college student
- Military status
- Felonies/Misdemeanors
- Health Care License infraction
- Match information
- NRMP participation
- Couples Match
- Academic history
- College(s) attended
- Medical school attended
- Medical school release
- USMLE and COMLEX scores
- Interruptions in medical school education
- Residencies & fellowships
- Supporting information
- Experiences & activities
- Employment (non-medical)
- Publications/presentations
- Honor societies/honors & awards
- Hobbies & interests
- Optional reflective statement
- Personal statement
- Medical school transcript
- Medical Student Performance Evaluation (MSPE or Dean's Letter)
- Photo
- Program Materials
- Evaluations/Letter(s) of Recommendation
- Program signals
Personal Information
This section is where you enter your basic demographic, biographic, and background information, including military service obligations, couples matching information, language proficiency, prior misdemeanors/felonies, and health care license infraction information.
Applicants also have the opportunity to share attributes that residency programs may identify as impactful, such as identifying themselves as a Pell Grant recipient or as a first-generation college student.
Geographic Connections
New to the 2025-2026 residency application cycle is the addition of "Geographic Connections." This section allows you to indicate up to three locations where you have a particularly strong connection. It can be (but doesn't have to be) where you grew up or lived for a period of time and can be different from your current address as collected in the "Contact Information" section. Note: It can also be somewhere you have not lived but where you may have a personal tie, such as where your significant other's family or other social support system may be located. Applicants will also be able to provide an optional, very brief explanation of why they have selected each geographic connection.
NRMP ID
Registering for the NRMP Match is a separate process from creating and submitting your ResidencyCAS application. You must go to the NRMP website (www.nrmp.org) to register and pay the one-time fee for the NRMP Match. Key points to remember:
- NRMP Match ID registration historically does not open until mid-September, and late registration for an additional fee begins after late January.
- You do NOT need your NRMP ID number to submit and certify your ResidencyCAS application.
- Your NRMP ID will automatically link to your ResidencyCAS account and be available to the programs where you apply. No manual entry is required.
Couples Match: Discuss with your advisors and partner if you will disclose your couples match status on ResidencyCAS. You are not required to disclose, and there are pros and cons to disclosure. In a survey of EM PDs, most responded that they contact the PD from the corresponding residency program at their institution when considering a member of a couple.5 Disclosing couples match status allows program directors from each specialty to lobby for their applicant's partner. Conversely, if a partner is applying to a specialty that is not offered at the same institution, some PDs may think the interview might be low-yield. When it comes to EM-EM couples, many programs may make extra efforts to interview both members of a couple if the status is disclosed, but a handful of programs may want to avoid EM-EM couples. In general, the attitude within the EM community is that the benefits probably outweigh the risks for most couples.
At-Risk Candidates: Applicants are required to disclose a history of felony or misdemeanor convictions. An applicant with this history is best served by accepting responsibility, taking ownership of what happened, and demonstrating conscious changes for the better. If an applicant selects "yes" in this section, a text box will pop up to provide an opportunity to offer clarifying information and context.
Academic History
In this section, you will enter information about the college(s) and medical school(s) you attend(ed) and any residencies or fellowships in which you may have already participated.
You will also have the opportunity to disclose interruptions in your medical school education with the requirement to select a reason for the gap (academic, financial, medical, research, personal, other) and the option to provide additional details for the interruption (up to 250 characters).
You can choose whether to release your application and interview offer information to your medical school. We recommend that you choose to do so, as this information allows your deans and advisors to view your progress through application season, including any interview offers received. This transparency with your medical school can help them guide you throughout the residency application process.
USMLE or COMLEX Transcripts
Within the ResidencyCAS platform, you will be directed on how to authorize and release your Step/Level scores. For the 2025-2026 application cycle, to upload USMLE scores, you will be directed to the Federation of State Medical Boards (FSMB) site to pay a one-time transcript fee. For COMLEX, you will enter your NBOME ID and pay your transcript fee directly within ResidencyCAS. You can track the status of your transcript request in the USMLE and COMLEX scores section of ResidencyCAS.
- Note: If your Step 2 score is not available at the time of your initial application, you must go back into this section of ResidencyCAS when the score is available and select "Re-Request."
Guidance about when to take USMLE Step 2 CK can be found in Chapter 3: Third Year and Planning for Fourth. Information about how your USMLE/COMLEX scores should influence your application strategy can be found in Chapter 8: Apply Smarter, Not Harder: Understand Your Competitiveness.
Osteopathic Candidates: You can upload COMLEX transcripts, USMLE transcripts, or both. If uploading COMLEX transcripts, you must authorize their release and pay a transcript fee, similar to the process for uploading USMLE scores. As mentioned in Chapter 2: The Preclinical Years, acceptance of COMLEX Level 1 may change with USMLE Step 1 and COMLEX Level 1 now being pass/fail examinations, but that is still unknown. Available data indicate that if you are an osteopathic medical student, taking at least USMLE Step 2 in addition to COMLEX Level 2 will open more opportunities for residency interviews.6 Refer to EMRA Match for programs that will accept COMLEX scores alone to help inform your application decisions.7
IMG Students: USMLE transcripts for IMGs are released by ECFMG rather than NBME.
Supporting Information
Experiences and Activities
You will be limited to 12 total experiences and will have the opportunity to choose your top three most meaningful/impactful experiences. For each experience, you will be asked to provide a brief description that explains your key responsibilities (600 characters), as well as information about the amount of time dedicated to the experience (Start/End Date and hours per week) and if the experience is ongoing.
For each of these experiences, you will assign a:
- Type: Work, Research, Volunteer/Service, Advocacy, Military Service, Teaching/Mentoring, Extracurricular Activity or Club
- Domain: Athletics, Clinical Informatics, Communication and Population Health, Customer Service, Direct Patient Care, Diversity and Equity, Global Health, Healthcare Administration, Leadership, Health Policy, Medical Education, Music/Art, Patient Safety, Public Health, Quality Improvement, Rural Health, Social Justice/Advocacy, Technology, Wellbeing, Other
- Competency: Accountability/Conscientiousness, Conflict Resolution, Critical Thinking, Cultural Humility, Ethical Principles, Innovation, Interpersonal and Communication Skills, Leadership, Reflective Practice/Personal Growth, Resilience, Situational Awareness, Systems Thinking, Teamwork, Time Management, Other
The purpose of labeling the experience types, domains, and competencies is to allow applicants to delineate with more detail, but in more standardized terms, how they have spent their time. These fields will factor into the ResidencyCAS holistic scoring tool used by programs to help surface applicants whose interests align well with the program's focus or mission. Some experiences may cross multiple Types, Domains, or Competencies. Applicants should make selections they feel are most reflective of the experience. There is an option to select "Other" for experiences that applicants feel do not easily fit within any one of the provided competencies.
Holistic Scoring Tool
The holistic scoring tool is a calculator that assigns a score to each applicant applying to a particular program based on weights set by that program. The score is calculated using discrete data from that applicant's application. It is important to understand that the holistic scoring tool is not intended as a filter. It is designed to allow programs to surface applicants who align well with their mission and recruitment goals, yet they may have otherwise been overlooked.
There is no such thing as a perfect score, and an applicant's score at one program will be different from that same applicant's score at another program because each program will adjust its holistic score for attributes it seeks to identify. The holistic score is only one component of application review and does not take the place of a thorough review of your application that programs will continue to perform. Because the holistic score is a relative value and unique to each program, an individual applicant does not receive their score.
Dual Applicants: If you are dual applying to EM plus another specialty that also uses ResidencyCAS, you might need to carefully consider how best to allocate your experiences, since the same 12 will be seen by all programs across all specialties to which you apply.
While you can list any experience you choose, a general rule of thumb is to select experiences that demonstrate a reasonable amount of time and/or effort committed to that experience over "one-off" events. For EM, we cannot overemphasize how essential it is to be authentic to who you are and what is important to you (not what you think programs want to hear)!
Employment (Non-Medical)
New in the 2025-2026 residency application cycle, you will have the opportunity to separately include up to three non-medical employments in your application, which will not count toward your other 12 experiences. While not necessarily intuitive, non-medical work experience can communicate valuable information about an applicant, including experience with customer service and task-switching skills, among others.
Non-medical employment may explain gaps in your education or less robust extra-curricular experiences, can demonstrate commitment to an activity often of significant time and/or effort in addition to your education, and may also help programs understand your life experience and path to medicine.
Publications/Presentations
You may include up to 30 publications and 30 presentations in this section, but most applicants to EM won't have nearly that many.
Honor Societies/Honors and Awards
You will have the opportunity to signify participation in Gold Humanism Honor Society, Alpha Omega Alpha, and Sigma Sigma Phi in the "Honor Societies" section. You may list an unlimited number of honors or awards as well. We recommend refraining from listing clerkship honors, as these are viewable in other areas of your application.
Hobbies and Interests
You may list up to three hobbies and interests, along with a description.
Supporting Information Section: Summary
Taken in sum, the "Supporting Information" section allows you to describe accomplishments outside of the classroom/clerkships and highlight personal qualities not captured elsewhere in the application. This section is often thought of as the "X-factor" of your application and helps reviewers gauge how well you resonate with the program's values. It can be helpful to think of this section as evidence to support the narrative you will reference in your personal statement and interviews.
In this section, there is a real opportunity to stand out from other applicants. Simply listing your experiences does you a disservice – the application is much stronger if you include brief details of each activity to highlight your role. Describe what you learned from each experience, what new skill(s) you acquired, and/or how it made you a better person. Focus on writing more about the experiences that were the most significant to your personal and professional development. Take advantage of the "Hobbies and Interests" section; programs like to have a window into who you are outside of medicine, and it's frequently a great springboard for conversations during program interviews. You should be prepared to talk about anything you include in this section during an interview day.
A common pitfall in the Supporting Information section of the application is exaggerating the amount of time you committed to an activity or the scope of your role and responsibilities. Be truthful – always.
Latecomers: Include activities and accomplishments in other fields in your experiences on your CV if they are substantial. There are many paths toward EM, so leadership, work, and research in other specialty areas may still be relevant. Emergency medicine as a specialty requires a broad set of skills and interests.
Optional Reflective Statement
This optional statement provides an opportunity for applicants to describe unique life experiences they have encountered or overcome along their journey to residency that are not captured elsewhere in the application. It is designed to offer more perspective on you as a person; however, it is different from your personal statement, which should focus on the experiences and background that have drawn you to and prepared you for EM. What you choose to include here might have nothing to do with your decision to pursue EM but can give reviewers more of a full picture of who you are and what it has taken for you to get to this place in your training. This essay opportunity is not meant to discuss common hurdles overcome by many applicants, such as academic struggles. Programs expect that most applicants will leave this prompt blank, either because it does not apply to them or because they may not feel comfortable sharing such personal information. Remember that if you do choose to answer, it is "fair game" for your interviewer to ask about this topic.
Some thematic examples of the types of experiences previous applicants have included in the reflective statement:
- Family Background: being an immigrant and the obstacles this status may have presented, first-generation college student
- Financial Background: being from a low-income family or other financial struggles that may have impeded your journey to medicine
- Community Setting: growing up in an area with high poverty levels, facing food scarcity, or housing insecurity
- Other Life Circumstances: loss of a family member, health issues affecting you or a close family member, being the main caretaker for a sick loved one
Personal Statement
Personal statements can cause a high level of anxiety. How do you write a personal statement that effectively introduces you and captures your excitement about EM? What is the role of the personal statement? How does it differ from other parts of your application? How much will it matter?
A survey of EM residency directors showed the most influential components of residency applications are SLOEs, residency interviews, EM evaluations/grades, and clinical clerkship grades. The personal statement ranked below all of these components in importance.8
This is good news and bad news. A poorly written or otherwise bad personal statement likely has more potential to harm than a good personal statement has the potential to help. It is unlikely a great personal statement will make up for an otherwise poor application, but sometimes a great personal statement can tip the scales in your favor.
So, how do you write a good statement? Applicants typically begin by describing by what path they came to discover EM as the field for them. Then show (rather than tell) programs that you have the qualities to be a great resident by using examples from your experiences and achievements. Writing about how much you enjoy EM does not distinguish you from any other applicant; focus instead on what makes you unique. Describe the challenges you've faced to demonstrate your ability to persevere. Highlight how your previous experiences show your passions, values, and goals, and how you plan to channel these into your career. You don't need to go into every past experience; choose key examples that highlight who you are and amplify your narrative. Programs want to know if you will be a good fit with their program, so close by discussing what you are looking for in a residency program and what you want to gain from the next 3-4 years of your training.
Other essential facts that apply to all writing apply here, too.9 Edit your statement, put it away for a few days, and then edit it again with fresh eyes. Have advisors and friends read it as well to offer a fresh perspective. Make sure you correct all grammar and spelling mistakes. Although it is stressful, try to have some fun with the process. It is, by definition, the most personal part of the application. Allow yourself to reflect on what makes you you, and let that shine through.
Your personal statement is limited to 4,000 characters. As of the 2025-2026 residency application cycle, you can only create one personal statement for all programs to which you are applying in EM. You cannot personalize statements for individual programs. You will have the opportunity to signify interest in a particular program through "Program Signals" and a particular geographic location through "Geographic Connections."
At-Risk Candidates: Applicants with a facet of their application that is likely to be considered a red flag, such as a USMLE/COMLEX or course failure, a felony or misdemeanor conviction, a gap in their CV, etc., should use at least part of the personal statement to address these issues.10 The optional reflective statement may also be an appropriate place to address these topics. These components are likely the initial places a reviewer will look for an explanation. If they do not find one, there is little incentive for them to go any further in considering you for an interview. Take ownership of your past and do not make excuses. Articulate how you have emerged from your challenges better equipped for a career in EM. Most importantly, have your advisor read your statement and give you feedback.
Latecomers: The personal statement may be a good place to explain how you came to EM as a specialty, but keep it concise. Be sure your statement also shares experiences that convey the bigger picture of who you are and what you have to offer.
Dual Applicants: While you cannot create different personal statements for different programs, you can create and assign different personal statements to different specialties, which is important for students applying to both EM and EM-combined programs (which are considered separate specialties in ResidencyCAS) or a different specialty that also uses ResidencyCAS.
Medical Student Performance Evaluation (MSPE) – AKA The Dean’s Letter
The MSPE is not a letter of recommendation but rather an administrative summary of your performance throughout medical school, up to and including your clinical clerkships. It emphasizes strong attributes demonstrated throughout your medical education, highlights your accomplishments, and addresses any red flags or difficulties, including course remediation/failure or identifying any gaps in your medical school education. It also provides a summary of the narrative feedback from your clinical clerkships.
The MSPE traditionally includes your rank compared to your classmates, and this can help you gauge your competitiveness as an applicant; however, not all medical schools have a class ranking system. In this case, your school will indicate this in the MSPE. Check with your dean ahead of time to understand your institution’s process so you can better understand your competitiveness.
At-Risk Candidates: Be familiar with your MSPE so you can address any red flags, such as course failures, unexplained extensions or gaps, or professionalism issues in your personal statement and during your interviews. Take ownership of the issues, reflect upon what you have learned, and be ready to explain the changes you have made to ensure that the past will not repeat itself during residency. It can be beneficial to work with your letter writers to help address these potential red flags as well.
Latecomers: If you change specialties, be sure to update your dean as soon as possible. They may choose to emphasize different aspects of your strengths or accomplishments as they relate to EM in the MSPE.
Medical School Transcript
Your transcript is a list of your preclinical and clerkship grades. Your MSPE will provide more detailed information about your clerkship performance. While basic sciences grades have been ranked lower in terms of importance to residency programs, performance in required clinical clerkships is cited as being highly valued.8
Photo
While your photo does not need to be from a professional photographer, you do need to appear professional. Appropriate attire and posing/positioning matter. No selfies! While some programs may choose to blind your photo as part of their initial review, they will likely use your photo once they have met you at an interview, so they can best remember and keep track of each applicant.
Program Materials
Letters of Recommendation
ResidencyCAS allows you to submit a maximum of four Letters of Recommendation (LoRs) to each program, but it is not necessary to upload four. It is variable how many total letters a program will want before they consider an application to be complete enough to offer an interview, though some programs require three total letters, making this a good target number. In Chapter 5: Applying for Away Rotations, it was discussed that the eSLOE obtained at the end of each EM clerkship is the single most crucial component of your application.4,6,8 As a reminder, eSLOEs are obtained by completing EM clerkships at institutions that have an EM residency program. A total of only two EM rotations are typically recommended or required.11
While it can be to your advantage to have both eSLOEs uploaded by the time ResidencyCAS applications open for programs to review, it's not a deal-breaker. Many programs will still consider you with only one eSLOE at the time of their application review and interview offer, though the majority want to see a second eSLOE by the time of interviews and ranking. Refer to EMRA Match and program websites for eSLOE number requirements and preferences. A third eSLOE is rarely suggested but may be beneficial if you have academic red flags or had a challenging EM rotation.12
In addition to the two eSLOEs recommended from your clerkship experiences, you can add LoRs from other faculty members with whom you have worked closely, either in SLOE format or narrative format. You may request a SLOE from an EM faculty member who works at a hospital affiliated with an EM residency program (eSLOE for academic EM faculty), one at a hospital not affiliated with an EM residency program (SLOE for non-academic faculty), or a faculty member you worked with during an EM subspecialty rotation, such as ultrasound, EMS, pediatric EM, or toxicology (SLOE from an EM subspecialty rotation).
O-SLOEs (Off-Service Standardized Letter of Evaluation) can be used for non-EM clinical experiences, such as surgery or intensive care rotations.13
For letters reflecting a non-EM clinical experience, you should preferentially request that letter in O-SLOE format, as this carries slightly more weight than a standard narrative LoR.
For letters reflecting non-clinical experiences, such as letters from research mentors, medical school advisors, deans, or individuals with whom you’ve worked closely on important projects or initiatives, a traditional narrative format should be used – just realize this will likely carry less weight than a clinical LoR.
Within ResidencyCAS, you will have the ability to request an EM SLOE (which you should select for eSLOEs, SLOEs for non-academic faculty, EM subspecialty SLOEs, and O-SLOES) or an EM Narrative Letter of Recommendation.
For both options, you must enter the names and email addresses of your letter writers, whether or not you waive the right to view each LoR, and indicate whether or not you give permission for schools, programs, or sites to contact the evaluator. In general, applicants waive the right to review their LoRs, allowing letter writers to provide a candid assessment.
Once this request has been submitted, your letter writer will receive an email that directs them to either the CORD eSLOE website (if you requested a SLOE) or Liaison Letters (if you requested a narrative LoR), which is the ResidencyCAS evaluator portal. You will be able to monitor the status of your LoRs, which will be listed as requested, accepted, or complete in your applicant portal.
It is important to know that after four LoRs are assigned to a program and completed, you can no longer remove/add LoRs. Therefore, if you plan to perform a late EM rotation (September or later) but are counting on this rotation for an eSLOE, it is important to leave a LoR spot open for this eSLOE at the time of your initial application submission. Additional letters can be added as they become available, but do not delay submitting your applications while waiting for eSLOEs to be uploaded. While each student rotation is different, it is reasonable to expect that an eSLOE may take a few weeks after your rotation for the program to complete. Programs will often make extra efforts to decrease the turnaround time for rotations occurring in September and beyond.
You can have more LoRs uploaded to ResidencyCAS than you can assign to each program, and can choose to assign different letters to different programs. However, it is important to note that each program should preferentially receive your academic EM faculty group eSLOEs. Academic EM faculty group eSLOEs carry more credibility and weight than any other type of SLOEs.14
Latecomers: While studies show that letters from a physician in a specialty other than EM, even in O-SLOE format, carry less value than an EM eSLOE, these letters are still valuable, especially as you may have a mentor or advisor from a different specialty who has worked closely with you.8 You can consider including a non-EM LoR if you had a strong relationship with the writer and feel they can speak to attributes or qualities less described in your other letters. Be sure to leave room in ResidencyCAS to upload two eSLOEs, even if they will be uploaded after you submit your application.
Reapplicants to EM: If applying to EM after beginning a residency in another specialty, it is critical to include a supportive LoR from your current program director, describing your performance as a resident.
Program Signals
Program signals are a method by which applicants can indicate a strong interest in a program at the beginning of the application season, with the goal of increasing the likelihood of receiving an invitation to interview.
In the 2025-2026 cycle for EM, applicants will have the opportunity to submit five program signals, all of equal weight, and are advised NOT to signal home or away programs where they completed a visiting rotation, as these are often high-yield in terms of interview offers. You will assign these signals as part of your ResidencyCAS application.
Residency programs will be able to view your signal at the time of initial file review, once ResidencyCAS opens to programs. Programs have utilized the signal in a variety of ways:
- Part of a holistic approach to application review;
- As a tie-breaker between similarly-matched signaling versus non-signaling candidates;
- As a screening tool;
- As a tool to prioritize wait-list order;
- As a topic for discussion during interviews (an applicant may be asked to expand on their reasoning behind the signal; however, they should not be asked where else they may/may not have signaled, why they did not signal, or if they participated in signaling).
While signals are not intended to be used as part of the rank list discussion and preparation, it is important to note that 11% of surveyed EM PDs reported using program signaling for this purpose in the 2022-2023 application cycle.15
You might imagine that a program that only receives a handful of signals might incorporate this information differently into its review process than a program that receives hundreds of signals. A survey of EM PDs in the 2022-2023 application cycle revealed that as the proportion of signaled applications decreased, the likelihood of a program offering interviews to a signaling applicant increased (and vice versa).15
As one would imagine, as the number of signals received by a program increases, the relative signal value at that program will decrease. If an applicant doesn't have the strongest application, and they utilize all their signals at highly competitive or "reach" programs (which are likely to receive a large number of signals), then the emphasis behind that applicant's signal may be lost and therefore not best utilized for the highest gain.
Depending on an applicant's competitiveness, there may be utility in sending a signal to one or more "safety" or less competitive programs (again, assuming they actually want to be at that program), but there is no data to support this particular recommendation. The most important factor remains that the applicant should signal programs where they are truly interested in training and think they would be a good fit.
Emergency medicine data from recent Match cycles shows that the likelihood of receiving an interview was higher at a signaled program than at a non-signaled program.16 While sending a signal does not grant you an automatic interview, it is important to note that the opposite is also true – programs are still offering interviews to candidates who did not signal them.
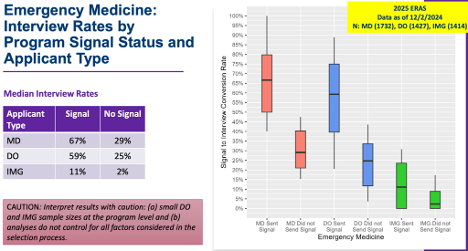
Figure 1. Emergency Medicine Applicant Interview Rates by Program Signal Status & Applicant Type, 2024-2025 cycle16 (used with permission)
Because signals will be assigned in concert with ResidencyCAS submission, it is strongly recommended that applicants spend some time researching programs and reflecting on what their priorities are in a prospective training program early, as they are putting together their initial application. There will be more opportunities to learn and reflect in depth on programs during the interview and ranking phase of the process, but having an understanding of some basic program information and the characteristics of applicants that have been accepted in the past is useful as applicants select the programs they plan to signal. There will not be a post-interview round of signals.
We strongly suggest that applicants work with their medical school and EM advisors and reflect honestly on the strength of their application. This, in turn, will help inform an applicant on the best allocation of their signals. We also suggest that applicants do their research and look closely at program information available to them via EMRA Match, Texas Star, the AAMC Residency Explorer tool, program websites, etc., to compare their application information with current/past residents. ResidencyCAS does allow programs to present some information as well as links to their website; however, it is not designed to replace the other tools above, which may be more useful in creating the list of programs to which you will apply.
Applicants with Limited Advising: Because the signaling process is still relatively new for EM, few emergency physicians outside of academics are aware of these changes to the residency application process, so they lack the necessary details to advise on signaling. Residency programs, on the other hand, are acutely aware of these changes as they affect them, too. Therefore, if your medical school is not affiliated with an EM residency program but you have contact with an advisor at an EM residency program outside of your institution, please reach out to them!
Note: If you are a student at a U.S. medical school and do not have access to any advisors at an EM residency program, you can email distanceadvising@cordjobboard.com to be connected with an advisor from an EM residency program.
The Bottom Line
- Be honest on your application; do not inflate your accomplishments or involvement in anything. Program directors look for congruence. They want to make sure the person they interact with on the interview day is consistent with the person they see on paper.
- Anything on your application is fair game to be discussed further in an interview. If it is on your application, be prepared to talk about it!
- Spelling and grammar errors can be a kiss of death. Spend time making your application clear, crisp, and error-free. From the ResidencyCAS site, you can print your application to review for errors. Have friends, family, and mentors read over your application before you submit it.
- Stick to the timeline. It is okay to not have two eSLOEs uploaded by the date ResidencyCAS opens to programs, but you must have your application (including other LoRs) submitted by this date. Do not submit late!
References
- Liaison International. ResidencyCAS Centralized Application Service. 2025.
- Council of Residency Directors in Emergency Medicine. Emergency Medicine Collaboration with ResidencyCAS. 2025.
- Liaison International. ResidencyCAS Applicant Help Center. 2025.
- King K, Kass K. What do they want from us? A survey of EM program directors on EM application criteria. West J Emerg Med. 2017;18(1):126-128.
- Council of Emergency Medicine Residency Directors Advising Students Committee in Emergency Medicine. (2018). [CORD ASC-EM Advising Addenda Study]. Unpublished raw data.
- National Resident Matching Program. Charting Outcomes: Program Director Survey Results, 2024 Main Residency Match. August 8, 2024.
- Emergency Medicine Residents’ Association. EMRA Match.
- Negaard M, Assimacopoulos E, Harland K, Van Heukelom J. Emergency Medicine Residency Selection Criteria: An Update and Comparison. AEM Educ Train. 2018;2(2):146-153.
- Olson DP, Oatts JT, Fields BG, Huot SJ. The residency application abyss: insights and advice. Yale J Biol Med. 2011;84(3):195-202.
- Graves AJ, Brown BM, Oller KL. To the Editor: Using the Personal Statement to Address Application Deficiencies. J Grad Med Educ. 2022;14(5):621.
- Hillman E, Lutfy-Clayton L, Desai S, Kellogg A, Zhang XC, Hu K, Hess J. Student-Advising Recommendations from the Council of Residency Directors Student Advising Task Force. West J Emerg Med. 2017;18(1):93-96.
- Love JN, Smith J, Weizberg M, et al. Council of Emergency Medicine Residency Directors' Standardized Letter of Recommendation: The Program Director's Perspective. Acad Emerg Med. 2014;21(6):680-687.
- Council of Residency Directors in Emergency Medicine. CORD Standardized Letter of Evaluation.
- Council of Residency Directors in Emergency Medicine, Advising Students Committee in EM. How to Get an Away Rotation Guide.
- Pelletier-Bui A, Fallon T, Smith L, et al. Program signaling in emergency medicine: The 2022-2023 program director experience. West J Emerg Med. 2024;25(5):715-724. doi:10.5811/westjem.19392
- Exploring the Relationship Between Program Signaling and Interview Invitations Across Specialties. Association of American Medical Colleges. December 2, 2024.