Ch. 4 - Finding Your Fit: Learning the Landscape of EM
One of the most exciting things about medicine is there is always more to learn. This is true for the application process as well. Now that you have decided on EM, the next thing you must consider is which type of residency will be best for you.
Factors Important for Residency Selection
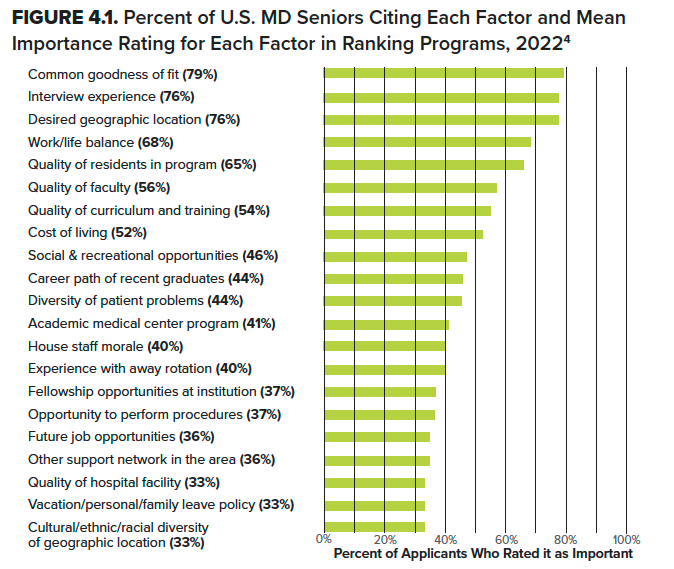
While all EM residency programs must meet the ACGME common and specialty-specific program requirements, there is still room for significant variation between programs. Students applying to EM say many factors are important in deciding where they apply and ultimately rank programs (see Figure 4.1).1-4 Many of these program attributes have been included as filter options in EMRA Match.
Location, Location, Location
Desired geographic location is typically the most important factor during both the application and ranking process. Some applicants want to be close to family, while others are looking to embark on a new adventure or seek unique social and recreational opportunities to enjoy when not at work. The cultural, racial, and ethnic diversity of the patient population may also vary by location. Residency programs in highly desirable urban areas will likely have a higher cost of living. Applicants with significant others may also need to consider the job opportunities available for their partners in each location. Of note, many physicians end up practicing in the same geographic location where they completed their residency training.5
Couples Match: Remember, you don’t have to match at the same institution to be within a certain geographic distance of each other. Target cities and geographic locations that have multiple residency programs in each of your specialties.
Osteopathic and IMG Candidates: Certain states and geographic regions have traditionally matched a higher number of osteopathic residents per program per year. The same holds true for IMG applicants.6 Of note, EMRA Match allows you to filter programs by the percentage of osteopathic and IMG residents they currently have in their program.
Comparing 3- and 4-Year Programs
One of the many things that makes EM unique is that applicants can apply to both 3- and 4-year training programs. Approximately one-fifth (19.4%) of programs are four years in length.2 Applicants must weigh the opportunity cost of spending an additional year being paid as a resident, rather than as an attending, with the benefits that can be gained from a 4-year training program.
Many applicants will apply to a mix of both 3- and 4-year programs and must consider what makes an additional year of training at each program “worth it.” For example, an extra year of training may provide additional opportunities to teach, develop experience in maintaining patient flow throughout the entire ED, provide EMS medical direction, allow for unique clinical rotations outside of the ED or within an EM subspecialty area, allow for participation in a longitudinal specialty track during residency (see the “Fellowships/Scholarly Tracks” section later in this chapter), and/or provide additional elective time to tailor your training experience to suit your individual needs. A 3-year program, meanwhile, allows you to enter fellowship training or work as an attending a year earlier.
Elective time is an opportunity to explore other areas within EM, especially if you have special interests like global health, medical education, simulation, research, wilderness medicine, wellness, administration, health equity, sports medicine, toxicology, EMS, or ultrasound. Elective experiences may help you decide about fellowship training, especially if you’re interested in a fellowship that is not available at your program.
Similarly, if you know you want to pursue a fellowship, a 3-year program might be beneficial to shorten your training years and save you a year. However, at the same time, a 4-year program could also be beneficial because it allows you to participate in more elective time during which you can pursue your interests, build your CV, or participate in a “fellowship track.”
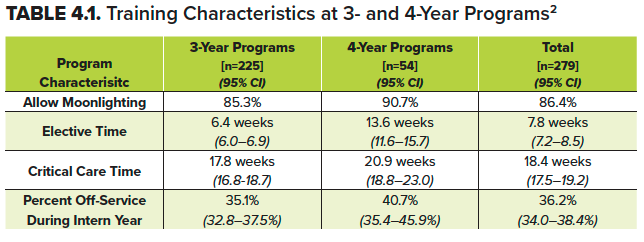
There is no significant difference in moonlighting opportunities, total critical care time, or percentage of time spent off-service during intern year between 3- and 4-year training programs; however, 4-year programs typically offer nearly 14 weeks of elective time, compared to only about six weeks of elective time at 3-year programs.2
Four-year programs are more likely to have internal medicine, neuro-ICU, and administration rotations, and on average have an additional 2.4 weeks of time spent doing pediatric EM.7
Training Environment
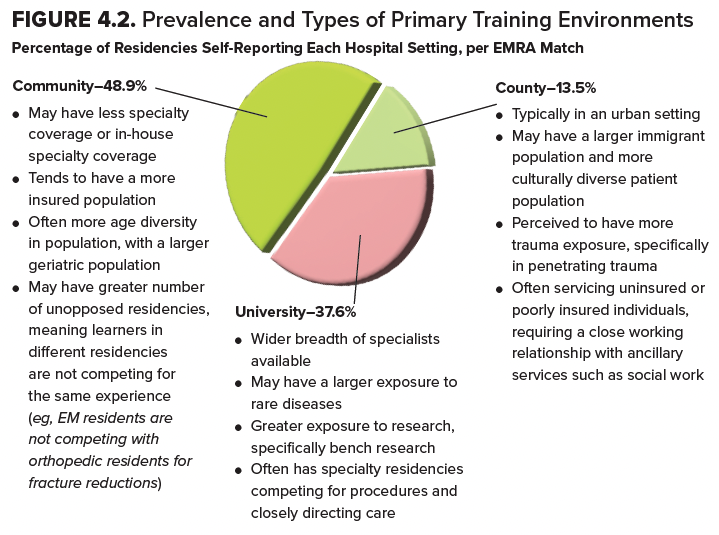
Every residency program is at a sponsoring institution that assumes ultimate responsibility for ensuring the program receives the support necessary to successfully train residents. This sponsoring institution is typically the primary clinical site where residents complete their training and may be a university, community, or county-based hospital (see Figure 4.3 for a breakdown of residencies by primary training environment). Many residency programs have additional sites to provide exposure to experiences not offered at the primary clinical site, such as community and rural sites, to expand learning environments and opportunities. There are pros and cons to each type of training environment. You should consider which learning environment will best prepare you for your ultimate career goals.
ED Patient Volume
While many applicants consider patient volume to be an important factor in choosing a residency program, this may or may not translate to increased learning opportunities. The ACGME requires the primary clinical site and any ED where a resident spends more than four months to have a minimum of 30,000 annual visits. The primary site should also see a minimum of 3% or 1,200 critically ill patients (whichever is greater).8 It can be important to explore the total number of critical care weeks vs. the general nature of those critical care experiences to ensure a robust exposure.
While some residency programs boast patient volumes in the hundreds of thousands, which may increase exposure to rare pathology, this may or may not hold true depending on the staffing models used at each program. Some residency training programs will be located at institutions that also train or employ non-physician providers (NPPs). The ability to work with and direct all layers of the patient care team is an important part of your practice. However, it is important to consider how working alongside NPPs in the ED during residency will affect your clinical practice and learning.
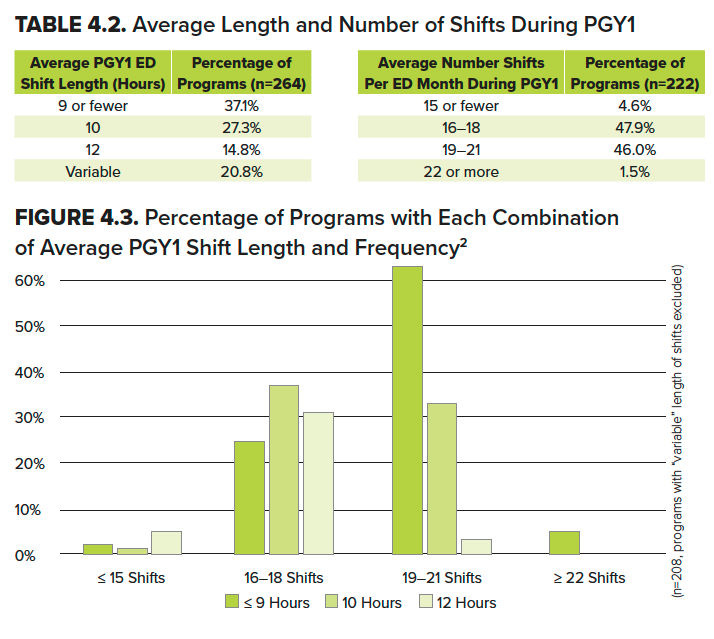
Work-Life Balance: Length and Number of Shifts Per Month
Per ACGME, EM residents may not work longer than 12-hour shifts in the ED. They must have a length of time off-duty that is equal to or longer than their scheduled shift length between each work period. Residents may not work for more than 60 scheduled hours per week seeing patients in the ED (and overall work no more than 72 total hours per week). EM residents must have at least 24 continuous hours off every seven days.8 Within these constraints, there is significant variability, though most programs require interns to work 16-21 shifts per month (of nine hours or less).2
Many residents cite time for personal and professional needs as key in preventing burnout. In one study, the authors found “when baseline needs of adequate sleep and self-care are not met, the capacity for self-actualization is limited. The strained, moment-to-moment mentality many residents experience does not permit introspection, processing of emotions, or learning from challenging patient encounters.”9
Seek enough clinical exposure to become clinically excellent, while maintaining your personal wellness and learning style. For example, those who learn best by seeing and doing may have a better educational experience at programs with more clinical duties, while those who learn best by reading and reflecting may be better suited to a program with more time for studying.
Program Size
The ACGME requires a minimum of 18 residents total per EM residency program to foster a sense of community and to ensure there is a critical mass of learners to support educational activities.8 The largest EM residency is a 4-year program that accepts 25 residents per year for a total of 100 residents. There is nothing inherently good or bad about a large or a small program. A smaller residency may have more dedicated one-on-one instruction and a closer-knit community, while a larger residency program may have greater resources, greater flexibility in scheduling, and more varied rotations. It is important to consider the number of clinical sites staffed by a program’s residents to understand how much actual opportunity for the interaction you will have with your colleagues while on shift. Additionally, as with every piece of “finding your fit,” it is important to consider what type of environment you thrive in — whether a smaller or a larger program.
Residency Program Culture
Each residency program will have a relatively unique culture that results from the personalities who work there and the program’s priorities. Which factors are overall most important in determining if you will be happy at the program? Which training environment do you think you will work and learn best in? Do you need a family-friendly program? Are you looking for a program that will push you to your clinical limits or one that will provide more time for pursuing research or other scholarly endeavors?
Arguably, this is the most important factor for any resident searching for their ideal program. You have already chosen the best field there is! You will likely get fabulous training among many of the programs you will be applying to. However, residency is hard — there are long hours, and it is emotionally, mentally, and physically draining. Finding the right colleagues and mentors to lean on is important. Program culture can be difficult to determine before interviewing. However, some sense of culture can be derived from each program’s profile on Facebook, Instagram, Twitter, and other social media platforms, as well as each program’s description of its culture on EMRA Match. Many programs have introduced Zoom “socials” that serve as a useful way to get a sense and feel for the culture at each program. The introduction of virtual socials provides opportunities to get more information about each program, meet current residents, and ask specific questions. Lastly, spending time with current residents while on rotation or during an in-person second look can give you a good “insider” perspective.
Moonlighting
Most EM residency programs (86%) allow residents to moonlight, either internally or externally.2 Moonlighting is permitted by the ACGME for non- PGY1 residents as long as it does not interfere with their education or cause a violation of duty hours. Internal moonlighting allows residents to work additional shifts within their training program, which provides them an opportunity to assume the mindset of independent practice while still working in a department alongside their regular faculty. External moonlighting opportunities may allow residents to work at urgent care locations or in rural, critical access hospitals where they may be the only physician for miles, stabilizing patients for transport to facilities with more advanced capabilities.
Compensation & Benefits
Residents of all specialties training at each sponsoring institution are paid on the same PGY pay scale. Nationwide, the average starting salary for interns across specialties is $64,200.10 While there may be mild salary differences between programs, given the regional variation in the cost of living, it is not recommended to make this a deciding factor in your rank list. Applicants may want to take note of additional benefits like meal plans, vacation time, parental leave policies, housing subsidies, insurance benefits, CME allowance, and retirement plans.
Original Research vs. Scholarly Activity Requirement
The ACGME requires resident and faculty involvement in scholarly activity in order to maintain accreditation. Historically, 39% of EM residency programs have mandated resident scholarly activity requirements to be fulfilled by original research.11 However, the 2022 ACGME Common Program Requirements allow trainees and their program directors to use a wide variety of options to fulfill scholarly activity requirements, including discovery, integration, application, and teaching.8,12 Applicants seeking to fulfill their scholarly activity requirements by writing textbook chapters, presenting at national conferences, curriculum development, national leadership positions, or non-peer-reviewed publications should pay attention to each program’s requirements.
Fellowships/Scholarly Tracks
If you are already interested in a fellowship, then attending residency at a program that offers your desired fellowship could be beneficial. You will likely have a better understanding of what the fellowship entails, plus the selection committee will already know you since they will have been your mentors during training. At the same time, it can also be nice to gain exposure to a different training environment by completing fellowship training in a new location. Fellowships can be, and are, entered both from 3- and 4-year programs.
For those who would like to begin developing a niche during residency, either in preparation for fellowship or to make themselves more marketable for a career in administration or academics, some programs offer scholarly tracks in areas such as medical education, administration, EMS, toxicology, ultrasound, and more. These tracks create mentorship communities within a residency program. Some programs require residents to participate in tracks, while others have optional tracks. A 2018 study found scholarly tracks led to higher rates of residents graduating into an academic career for many reasons, including high levels of mentorship, scholarship, and advanced training.13
Newer or Established Residency Programs
There is no data to suggest that a newer vs. established program will give you a better residency experience. However, there are pros and cons to consider. A newer program will likely have more leeway to incorporate new ideas and innovations, allowing residents to make a lasting contribution to the program. A more established program will have the advantage of being a known commodity, with a larger alumni network to access when searching for jobs, fellowships, or niche types of mentorship. It is important to keep an open mind, as either type of program may serve your needs as a trainee.
Reputation
Avoid picking a residency program based on “reputation.” There is no “best” residency program, only a set of programs that will be the best fit for you based on your future goals, learning style, and lifestyle. In September 2014, all major EM organizations wrote a co-signed letter to Doximity concerning the methodology behind its “Reputation” filter in their Residency Navigator tool.14 That faulty filter has been shown to cause one-quarter to one-half of applicants to influence their rank lists.15,16 Rely on objective data, rather than unvalidated “reputation rankings,” when comparing which program will best fit your needs.
Osteopathic Students: Historic/Ongoing Osteopathic Affiliation
Starting in 2020, all programs merged under a single GME accreditation system. If a student feels that maintaining an osteopathic-focused education is important, they can find historically AOA programs that have applied for ACGME “Osteopathic Recognition,” which conveys their distinction in educational programming.
Use search filters (percent osteopathic residents currently at the program, acceptance of COMLEX in lieu of USMLE, etc.) in addition to reviewing data on the ACGME website. EMRA Match also allows you to filter programs by the percentage of osteopathic residents they currently have in their program. Reviewing the degrees held by faculty members, either DO or MD, at different programs may be helpful as well. Remember, just because a program does not currently have an osteopathic resident, it does not eliminate your chances — but it can guide a realistic approach to applying.
The Bottom Line
- Start researching programs early to get a sense of what you find important in programs and which programs fit your needs.
- Multiple factors go into selecting a residency program. Only you can determine the program that is the best fit for you.
- Avoid relying on “reputation rankings” when considering which programs fit your needs.
References
- Jarou Z, Ochsenbein S, Franzen D, Fairbrother H, Kellogg A. CORD Research Abstracts 2016: Do Students Have Access to the Data They Desire When Selecting an Emergency Medicine Residency Program? West J Emerg Med. 2016; 17:S10-11.
- Emergency Medicine Residents’ Association. EMRA Match. https://webapps.acep.org/utils/spa/match#/search/map.
- National Resident Matching Program. Results of the 2017 NRMP Applicant Survey. http://www.nrmp.org/wp-content/uploads/2017/09/Applicant-Survey-Report-2017.pdf.
- National Resident Matching Program. Data Release and Research Committee: Results of the 2022 NRMP Applicant Survey. Washington, DC. 2022.
- Koehler TJ, Goodfellow J, Davis AT, Spybrook J, vanSchagen JE, Schuh L. Predicting In-State Workforce Retention After Graduate Medical Education Training. J Grad Med Educ. 2017;9(1):73-78.
- Kukulski P, Goode D, McEvoy B, Hay S, Ahn J. (2020). Geographic Trends in the Emergency Medicine Match. West J Emerg Med. 2020;21(4.1):S19.
- Gottlieb M, Arno K, Kuhns M, Chan TM. Distribution of Clinical Rotations Among Emergency Medicine Residency Programs in the United States. Acad Emerg Med. 2018;2(4):288-292.
- Accreditation Council for Graduate Medical Education (ACGME). ACGME Program Requirements for Graduate Medical Education in Emergency Medicine, 2022.
- Fortenberry K, Knox J, Van Hala S. What Do Residents Want for Burnout Prevention? … Time. Acad Med. 2018;93(3):343-344.
- Roberts R. Medscape Residents Salary & Debt Report 2022. Published July 29, 2022.
- Geyer BC, Kaji AH, Katz ED, Jones AE, Bebarta VS. A National Evaluation of the Scholarly Activity Requirement in Residency Programs: A Survey of Emergency Medicine Program Directors. Acad Emerg Med. 2015;22(11):1337-1344.
- Accreditation Council for Graduate Medical Education (ACGME). Specialty-Specific Program Requirements: Resident/Fellow Scholarly Activity, ACGME. 2022.
- Jordan J, Hwang M, Kaji AH, Coates WC. Scholarly Tracks in Emergency Medicine Residency Programs Are Associated with Increased Choice of Academic Career. West J Emerg Med. 2018;19(3).
- EM Coalition. Letter to Nate Gross, MD, Doximity. https://www.cordem.org/globalassets/files/board/adv.--position-statements/doximity-letter.pdf. Sept. 12, 2014.
- CORD Abstracts 2015. Effect of Doximity Residency Rankings on Residency Applicants’ Program Choices. West J Emerg Med. 2015;16(6):889-893.
- Peterson WJ, Hopson LR, Khandelwal S, et al. Impact of Doximity Residency Rankings on Emergency Medicine Applicant Rank Lists. West J Emerg Med. 2016;17(3):350-354.