Ch. 7 - Musculoskeletal Pain
Andrew K. Chang, MD, MS | Albany Medical Center
Acute musculoskeletal pain is an extremely common presenting condition seen in emergency practice. Just as the range of extremity injuries can vary from a simple contusion to an open fracture or dislocation, so too can the treatment options vary from simple over the counter analgesics to intravenous opioids, depending on the pain severity.
Although there has been a recent emphasis on the non-opioid pharmacologic management of pain,1 it is important to recognize that opioids are still an important as well as an appropriate treatment option, especially for severe pain presentations and those unremitting to other non-opioid alternatives. The focus of this chapter is on the safe and effective management of acute musculoskeletal extremity pain in the emergency setting.
Note: Because back pain is so common - the sixth most common principal reason for an ED visit2 - and often has specific treatment strategies not used in other types of musculoskeletal pain, it will be discussed in a separate chapter.
NON-OPIOID ORAL ANALGESICS
Patients presenting with a mild to moderate extremity injury can often be managed with non-opioid analgesics, including nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, naproxen, ketorolac, and diclofenac among others (see Table 1 for a listing of commonly used NSAIDs). NSAIDs are considered the first-line treatment regimen for presentations of mild to moderate acute pain and can be administered orally (PO), intravenously (IV), intramuscularly (IM), per rectum (PR), or topically. For patients who have attempted over the counter analgesics before ED arrival, it is important to ask both the dose and time last taken, as many patients may have taken a subtherapeutic dose and may benefit from additional dosing while in the ED. In the case of NSAIDs, there is no difference in efficacy or time to onset of oral ibuprofen when compared to parenteral ketorolac,3 so unless the patient is unable to tolerate oral medication the oral route is generally preferable. Ketorolac and ibuprofen are two of the most commonly used NSAIDs, and some research has suggested that the analgesic ceiling is 400mg for oral ibuprofen and 10 mg for IV ketorolac.4,5 An ED-specific study also concluded that 400 mg PO was the analgesic ceiling for ibuprofen for short-term pain relief among adults presenting to the ED with acute pain.6 A systematic review found 400 mg ibuprofen was superior to 1,000 mg acetaminophen for acute pain relief but noted that the combination of both ibuprofen and acetaminophen was superior to either analgesic agent alone.7 It is important to note this research was based on dental pain management and may not apply to all musculoskeletal pain presentations. For mild acute pain, ibuprofen is dosed at 400 mg every 4-6 hours as needed with a maximum dose of 3,200 mg per day.
Not all NSAIDs have the same pharmacokinetic properties, which may result in clinically relevant differences in response depending on the specific patient and pain pathology.8 If a patient lacks a sufficient analgesic response to one NSAID class, one may consider trying an alternative class at a comparable effective dose (see table 1 for a list of common NSAID analgesics used for musculoskeletal injuries in the emergency setting). NSAIDs should be used cautiously among adults with cardiovascular comorbidities, volume depletion, pre-existing renal or liver disease, peptic ulcer disease, or loop diuretic use as these place patients at higher risk of drug-induced acute renal failure.9 For gastric prophylaxis, consider administering a proton pump inhibitor (PPI) when treating with an NSAID in an older adult.10 NSAIDs also carry an increased risk of major adverse cardiovascular events (MACE) and disrupt the protective cardiovascular effects of aspirin.11,12 This increased risk has been demonstrated in patients with and without a history of coronary artery disease (CAD) when NSAIDs were taken for at least a 7-day duration.12,13 Even short-term use of NSAIDs has been associated with recurrent myocardial infarctions and death.14
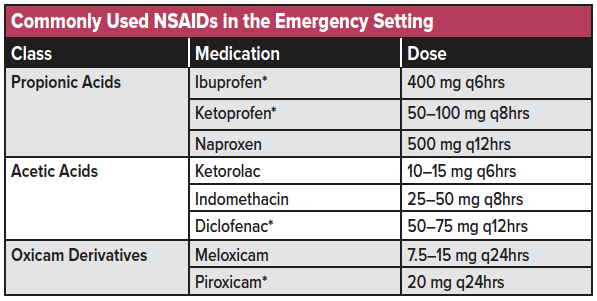
(*available in topical formulations)
NSAIDs are generally thought to be more effective than acetaminophen for acute pain. However, the latter is a reasonable option among patients with mild to moderate pain or among patients who are either allergic or have a sensitivity (eg, gastric upset) to NSAIDs. Acetaminophen 500-975 mg orally every 4-6 hours is considered a safe initial treatment for common mild to moderate pain ailments, though the manufacturer of Tylenol recently lowered the maximum recommended daily dose to 3 g instead of 4 g. In a trial of over 400 non-elderly adult patients presenting to the ED with an acute extremity injury, patients were randomized to ibuprofen (400 mg)/acetaminophen (1,000 mg), oxycodone/acetaminophen (Percocet©), hydrocodone/acetaminophen (Vicodin©), or codeine/acetaminophen (acetaminophen with codeine #3©).15 At both one and two hours, there was no difference in pain relief among the four groups, including among a subgroup of patients with confirmed fractures on radiography and those presenting with “10 out of 10” pain intensity. Although the results of this study imply that most acute extremity injuries can be managed in the ED with a combination of non-opioid analgesics, it needs to be emphasized that the lack of a difference is an average and that any individual patient might receive better pain relief with a particular analgesic, including an opioid. In other words, that which is generally true among a studied population may not apply to every single individual patient, thereby emphasizing the importance of clinical judgment when treating the patient in front of you. An example of a patient requiring a stronger analgesic regimen would be a patient with a displaced fracture that required a closed reduction to realign bony segments.
TOPICAL ANALGESICS
For certain injuries, such as sprains and muscle pulls/muscle strains, the use of topical analgesics such as diclofenac, ketoprofen, ibuprofen, 4-5% lidocaine patch, EMLA cream, and capsaicin cream may be used in conjunction with oral or parenteral analgesics and may even be sufficient as a primary treatment. Topical analgesics come in variations such as gels, creams, sprays, or plasters, though evidence suggests that gels are the most effective formulation.16 A 2017 Cochrane review showed gel formulations such as diclofenac, ibuprofen, and ketoprofen resulted in statistically significant improvements in pain relief among those with acute musculoskeletal pain. However, comparisons of topical and oral analgesics were rare.16 Topical analgesics should be applied to unbroken skin and should not be used with heating pads, which may cause excessive absorption. Patients should be warned to avoid contact of the topic analgesic with mucous membranes and be advised to use gloves during the application process.
REGIONAL NERVE BLOCKS
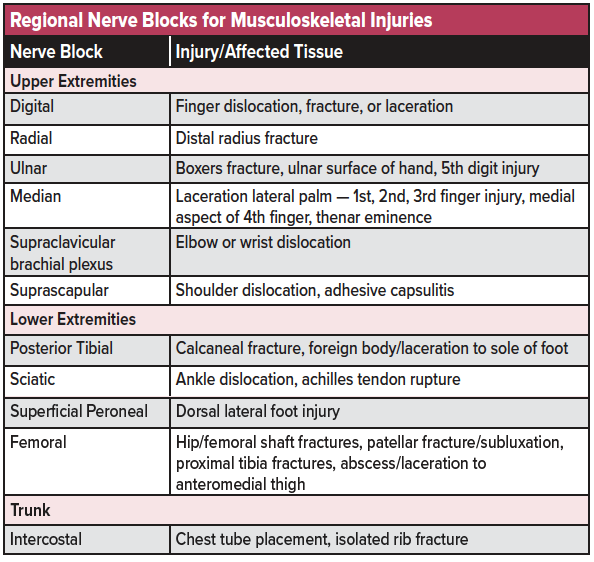
Nerve blocks provide the advantage of a localized form of pain relief, improved door-to-analgesia timing, and lowered doses of overall analgesic medication.17-19 See table 2 for a list of commonly used nerve blocks for musculoskeletal injuries in the emergency setting. Nerve blocks using common anesthetics (eg, lidocaine, bupivacaine, ropivacaine) can be used as a stand-alone analgesic modality, though optimally are used as part of a multimodal analgesic regimen or as a bridge to further inpatient pain management.20 Compared to other emergency procedures, nerve blocks are relatively easy to learn and can be effectively utilized at the residency level with proper training.21 Ultrasound-guidance provides further safety and efficacy in administering nerve blocks.22 See the chapter on Ultrasound-Guided Nerve Blocks for further discussion on how to perform these procedures.
KETAMINE
Subdissociative dose ketamine (0.1-0.3 mg/kg IV) has been shown to provide analgesic effect while preserving airway reflexes, spontaneous respiration, and cardiopulmonary stability among non-elderly adults.23 A recent systematic review and meta-analysis showed that low dose intravenous ketamine provides analgesia comparable to that of intravenous morphine at 0.1 mg/kg.24 However, it is unclear whether ketamine is effective beyond an initial dose.25 Among older patients aged 65 years and older, 0.3 mg/kg IV SDK administered slowly over 15 minutes offers analgesic efficacy comparable to morphine in the treatment of acute moderate/severe pain, though with an increased incidence of dose-dependent adverse events,26 including a feeling of unreality, sedation, nausea, vomiting, dizziness, and nystagmus (seen shortly after onset). These adverse effects have been shown to decrease in frequency when subdissociative dose ketamine was administered as a slow infusion over 10-15 minutes rather than as a bolus.23
NITROUS OXIDE
Nitrous oxide (N2O), or laughing gas, is an odorless and non-irritating inhaled analgesic with fast-onset and short duration.27,28 N2O is believed to function as an NMDA-R antagonist (similar to ketamine).29 N2O is commonly administered as a 50:50 N2O: Oxygen concentration30 with short onset (3-5 min)28 and rapid (3-5 min) recovery following discontinuation.28 N2O is a useful alternative when IV access is undesired or difficult to attain. To avoid complications, it is recommended to administer N2O under continuous cardiac monitoring in a setting where airway management is available.31
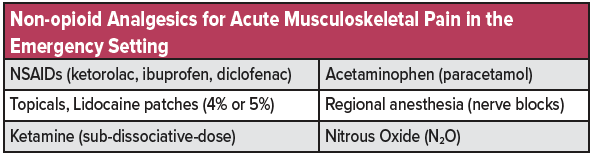
See table 3 for a list of commonly used non-opioid analgesics used for musculoskeletal injuries in the emergency setting.
OPIOID ANALGESIA
If a patient is deemed to require the use of oral opioids to manage an acutely painful injury, a series of ED-based studies have shown no difference in efficacy among oral formulations such as oxycodone/acetaminophen, hydrocodone/acetaminophen, and codeine/acetaminophen in the treatment of acute extremity pain.15,32,33 Although codeine, which is metabolized to morphine, is a schedule III narcotic (implying less addictive potential than schedule II narcotics, such as oxycodone and hydrocodone), one should be aware that patients may demonstrate significant variability of codeine metabolism. Codeine itself is a pro-drug with analgesic effects dependent on the metabolic conversion from the pro-drug form to codeine-6-glucuronide and morphine by the liver CYP450 enzyme (CYP2D6). This enzymatic reaction has significant allelic variability.34,35 Both poor metabolizers as well as and ultrarapid metabolizers exist among the population, with up to 10% of the population lacking the enzyme necessary for codeine conversion and 1-7% of the Caucasian population being ultra-rapid codeine metabolizers.34,36 This variation results in uncontrolled and unpredictable variability in analgesic response making codeine less desirable than other safer formulations that are available.
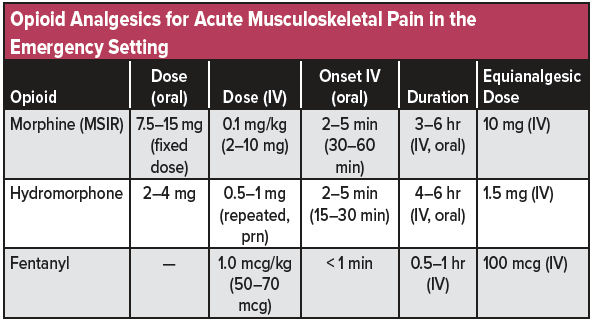
Patients with moderate to severe acute pain, such as from open or severely displaced fractures or joint dislocations, may require the use of intravenous opioids. Common opioids options include morphine 0.1 mg/kg IV, hydromorphone 0.5–1.0 mg IV, and fentanyl 1 mcg/kg IV (see table 4 for a list of commonly used opioid analgesics used for musculoskeletal injuries in the emergency setting). Pain unexpectedly requiring large amounts of intravenous opioids should result in consideration of alternative pathologies, such as acute compartment syndrome or neurovascular injury.
*For opioid-naïve patients, it is strongly recommended to start with smaller doses of opioids, such as hydromorphone 0.5 mg IV, but frequently reassess and re-dose as needed in order to avoid undertreatment of pain while monitoring for adverse effects. Repeat doses of hydromorphone (1mg IV) have been shown to be safe in patients with moderate to severe acute pain37 and often required in patients with higher opioid-tolerance38 emphasizing the importance of early reassessment for analgesic optimization.
MUSCULOSKELETAL PAIN DISPOSITION
In general, most patients with musculoskeletal pain will be discharged from the ED. For these patients it is important to emphasize the use of basic non-pharmacologic therapies when possible, such as the commonly used mnemonic “RICE”: R= rest (ie, use of crutches, sling, etc.), I=ice, C=compression (ie, ACE™ wrap, air-cast ankle stirrup), E=elevation (eg, elevating lower extremity when not ambulating). Emphasizing these non-pharmacologic therapies, along with setting realistic patient expectations, should allow for management with non-opioid analgesics such as prescription-strength ibuprofen even if the patient initially received opioids while in the ED. While the ultimate goal of pain management is to improve quality of life by returning patients to their baseline functional status, immediate elimination of all pain is likely not feasible. The goal is to reduce pain intensity to allow patients to continue their daily activities as their painful condition gradually heals.39 As the aforementioned study showed no difference between a combination of ibuprofen and acetaminophen against three commonly used opioids while in the ED,15 it is not unreasonable to think that this regimen will also be effective after ED discharge, since the natural history of most injuries is to improve and the healing process will likely be accelerated when combined with the non-pharmacological therapies mentioned earlier (ie, “RICE”). If the patient is unable to successfully fill their prescription, consider discharging them with a “starter pack” of ibuprofen/acetaminophen to ensure analgesic availability.
For those patients in whom the decision to prescribe opioids upon ED discharge has been made, the CDC guidelines state that three days or less will often be sufficient and that more than seven days will rarely be needed.40 Although not specifically studied, the author often instructs patients to use prescription-strength ibuprofen preferentially and taper the number of opioid tablets used each day if prescribed.
Patients may require admission to the hospital for intractable pain, intractable vomiting, social reasons (eg, older woman with both concomitant ankle and wrist fractures preventing the use of walker/crutches/cane), or operative intervention. Such patients may require intravenous analgesics initially and then are gradually transitioned to oral analgesics prior to discharge by the inpatient team.
SUMMARY
Musculoskeletal pain pathology is a common presenting complaint in the emergency setting. However, a combination of both opioid and non-opioid analgesics combined as part of a multimodal approach to pain management can effectively treat these painful conditions. Consider topical analgesics and nerve blocks as adjuncts to the traditional oral and parenteral regimen. Emphasize that the goal is not zero pain, but tolerable pain that allows patients to continue their daily activities during a painful condition. Patients often may be discharged on a short course of combination oral ibuprofen and acetaminophen. For more severe pain, a short course of oral opioids may be considered with recommendations to taper daily.
References
- Poon, S.J., and M.B. Greenwood-Ericksen, The opioid prescription epidemic and the role of emergency medicine. Ann Emerg Med, 2014. 64(5): p. 490-5.
- Rui, P., K. Kang, and J. Ashman National Hospital Ambulatory Medical Care Survey: 2016 emergency department summary tables. 2016.
- Turturro, M.A., P.M. Paris, and D.C. Seaberg, Intramuscular ketorolac versus oral ibuprofen in acute musculoskeletal pain. Ann Emerg Med, 1995. 26(2): p. 117-20.
- Seymour, R.A., P. Ward-Booth, and P.J. Kelly, Evaluation of different doses of soluble ibuprofen and ibuprofen tablets in postoperative dental pain. Br J Oral Maxillofac Surg, 1996. 34(1): p. 110-4.
- Motov, S., et al., Comparison of Intravenous Ketorolac at Three Single-Dose Regimens for Treating Acute Pain in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med, 2017. 70(2): p. 177-184.
- Motov, S., et al., Comparison of Oral Ibuprofen at Three Single-Dose Regimens for Treating Acute Pain in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med, 2019.
- Bailey, E., et al., ibuprofen and/or paracetamol (acetaminophen) for pain relief after surgical removal of lower wisdom teeth. Cochrane Database Syst Rev, 2013(12): p. CD004624.
- Pescatore, R. When Ibuprofen Fails, Naproxen Isn’t the Answer. Emergency Medicine News, 2018. 40, 10.
- Aalami, O.O., et al., Physiological features of aging persons. Arch Surg, 2003. 138(10): p. 1068-76.
- Pilotto, A., et al., Proton-pump inhibitors reduce the risk of uncomplicated peptic ulcer in elderly either acute or chronic users of aspirin/nonsteroidal anti-inflammatory drugs. Aliment Pharmacol Ther, 2004. 20(10): p. 1091-7.
- American College of Rheumatology Ad Hoc Group on Use of, S. and D. Nonselective Nonsteroidal Antiinflammatory, Recommendations for use of selective and nonselective nonsteroidal antiinflammatory drugs: an American College of Rheumatology white paper. Arthritis Rheum, 2008. 59(8): p. 1058-73.
- Danelich, I.M., et al., Safety of nonsteroidal antiinflammatory drugs in patients with cardiovascular disease. Pharmacotherapy, 2015. 35(5): p. 520-35.
- Gislason, G.H., et al., Risk of death or reinfarction associated with the use of selective cyclooxygenase-2 inhibitors and nonselective nonsteroidal antiinflammatory drugs after acute myocardial infarction. Circulation, 2006. 113(25): p. 2906-13.
- Schjerning Olsen, A.M., et al., Duration of treatment with nonsteroidal anti-inflammatory drugs and impact on risk of death and recurrent myocardial infarction in patients with prior myocardial infarction: a nationwide cohort study. Circulation, 2011. 123(20): p. 2226-35.
- Chang, A.K., et al., Effect of a Single Dose of Oral Opioid and Nonopioid Analgesics on Acute Extremity Pain in the Emergency Department: A Randomized Clinical Trial. JAMA, 2017. 318(17): p. 1661-1667.
- Derry, S., et al., Topical analgesics for acute and chronic pain in adults - an overview of Cochrane Reviews. Cochrane Database Syst Rev, 2017. 5: p. CD008609.
- Johnson, B., et al., Door-to-block time: prioritizing acute pain management for femoral fractures in the ED. Am J Emerg Med, 2014. 32(7): p. 801-3.
- Wilson, C., Feeling Blocked? Another Pain Management Tool in the Emergency Department. Ann Emerg Med, 2018.
- Beaudoin, F.L., et al., Ultrasound-guided femoral nerve blocks in elderly patients with hip fractures. Am J Emerg Med, 2010. 28(1): p. 76-81.
- Hards, M., et al., Efficacy of Prehospital Analgesia with Fascia Iliaca Compartment Block for Femoral Bone Fractures: A Systematic Review. Prehosp Disaster Med, 2018. 33(3): p. 299-307.
- Akhtar, S., et al., A brief educational intervention is effective in teaching the femoral nerve block procedure to first-year emergency medicine residents. J Emerg Med, 2013. 45(5): p. 726-30.
- Neal, J.M., Ultrasound-Guided Regional Anesthesia and Patient Safety: Update of an Evidence-Based Analysis. Reg Anesth Pain Med, 2016. 41(2): p. 195-204.
- Motov, S., et al., A prospective randomized, double-dummy trial comparing IV push low dose ketamine to short infusion of low dose ketamine for treatment of pain in the ED. Am J Emerg Med, 2017. 35(8): p. 1095-1100.
- Karlow, N., et al., A Systematic Review and Meta-analysis of Ketamine as an Alternative to Opioids for Acute Pain in the Emergency Department. Acad Emerg Med, 2018. 25(10): p. 1086-1097.
- Kirschner, J.M. and B.R. Hunter, Is Low-Dose Ketamine an Effective Alternative to Opioids for Acute Pain? Ann Emerg Med, 2019. 73(5): p. e47-e49.
- Motov, S., et al., Intravenous subdissociative-dose ketamine versus morphine for acute geriatric pain in the Emergency Department: A randomized control trial. American Journal of Emergency Medicine, 2018.
- Huang, C. and N. Johnson, Nitrous Oxide, From the Operating Room to the Emergency Department. Curr Emerg Hosp Med Rep, 2016. 4: p. 11-18.
- Pasaron, R., et al., Nitrous oxide procedural sedation in non-fasting pediatric patients undergoing minor surgery: a 12-year experience with 1,058 patients. Pediatr Surg Int, 2015. 31(2): p. 173-80.
- Jevtovic-Todorovic, V., et al., Nitrous oxide (laughing gas) is an NMDA antagonist, neuroprotectant and neurotoxin. Nat Med, 1998. 4(4): p. 460-3.
- American Society of Anesthesiologists Task Force on, S. and N.-A. Analgesia by, Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology, 2002. 96(4): p. 1004-17.
- Babl, F.E., J. Grindlay, and M.J. Barrett, Laryngospasm With Apparent Aspiration During Sedation With Nitrous Oxide. Ann Emerg Med, 2015. 66(5): p. 475-8.
- Chang, A.K., et al., Comparative Analgesic Efficacy of Oxycodone/Acetaminophen vs Codeine/Acetaminophen for Short-Term Pain Management Following ED Discharge. Pain Med, 2015. 16(12): p. 2397-404.
- Chang, A.K., et al., Comparative Analgesic Efficacy of Oxycodone/Acetaminophen Versus Hydrocodone/Acetaminophen for Short-term Pain Management in Adults Following ED Discharge. Acad Emerg Med, 2015. 22(11): p. 1254-60.
- Heiskanen, T., K.T. Olkkola, and E. Kalso, Effects of blocking CYP2D6 on the pharmacokinetics and pharmacodynamics of oxycodone. Clin Pharmacol Ther, 1998. 64(6): p. 603-11.
- Smith, H.S., Opioid metabolism. Mayo Clin Proc, 2009. 84(7): p. 613-24.
- Eichelbaum, M. and B. Evert, Influence of pharmacogenetics on drug disposition and response. Clin Exp Pharmacol Physiol, 1996. 23(10-11): p. 983-5.
- Chang, A.K., et al., Safety and efficacy of rapid titration using 1mg doses of intravenous hydromorphone in emergency department patients with acute severe pain: the “1+1” protocol. Ann Emerg Med, 2009. 54(2): p. 221-5.
- Chang, A.K., et al., Randomized clinical trial of the 2 mg hydromorphone bolus protocol versus the “1+1” hydromorphone titration protocol in treatment of acute, severe pain in the first hour of emergency department presentation. Ann Emerg Med, 2013. 62(4): p. 304-10.
- Lee, T.H., Zero Pain Is Not the Goal. JAMA, 2016. 315(15): p. 1575-7.
- Dowell, D., T.M. Haegerich, and R. Chou, CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016. JAMA, 2016. 315(15): p. 1624-45.