Ch. 1 - Pain Recognition & Assessment
David H. Cisewski, MD, MS | Icahn School of Medicine at Mount Sinai
Sergey M. Motov, MD, FAAEM | Maimonides Medical Center
Pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage.1
In a broader and clinically applicable definition, pain can be classified as acute, chronic, or acute on chronic. Pain can be described as dull, aching, throbbing, stabbing, burning, "worst of my life," or completely out of proportion to the physical exam. Pain is unique to the individual, subjective, and may be difficult to describe. From the patient’s perspective, pain can be confusing, unrelatable, and uncontrollable. If left undiagnosed and untreated, pain can become chronic, crippling, and all-consuming.
From the perspective of the emergency care provider, pain is the unrelenting, unremitting focus of every shift for the vast majority of patients. Pain affects every age, gender, and ethnicity and can vary in presentation based on each of these patient characteristics. Pain can be associated with pathology in nearly every organ, system, and disease process. Pain is the single most common presenting symptom in the emergency department, ranging between 75-80% of all chief complaints.2 With current estimates of 137 million emergency room visits in the U.S. per year, over 100 million patients requiring attention for pain of different levels of severity.3
Importantly, pain is a symptom, not a diagnosis. The challenge of the emergency care provider is to recognize, understand, and effectively treat this pain. Though emergency care clinicians become skilled at identifying and considering the pain - identifying and managing life-threatening diagnoses - they often waver in balancing pain relief against the unwanted and dangerous adverse effects of various medications.
OLIGOANALGESIA IN THE EMERGENCY SETTING
"Oligoanalgesia" refers to the undertreatment of pain. Main causes of the undertreatment include an underestimation of pain, incorrectly dosed analgesia, or delayed analgesic delivery. However, the reason for the undertreatment of pain is multifactorial and involve both the provider and the patient (see tables).7-10
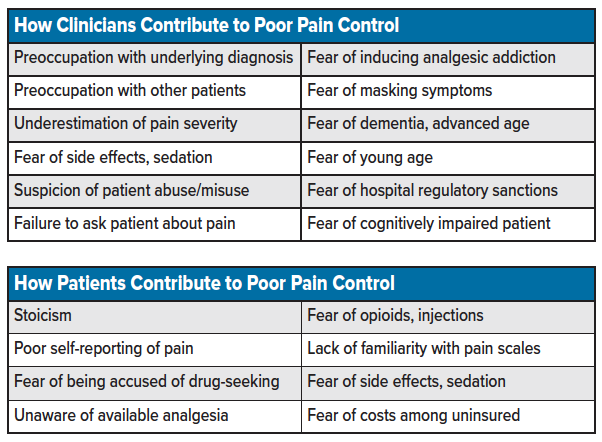
Pain is a dynamic entity characterized by a physiologic and neurologic response, compounded by socioeconomic status, past experiences, comorbidities, cultural and personal beliefs. That is, pain is an experience unique to the individual encountering it. Pain can be accentuated by fear and anxiety or suppressed by the fear of seeking treatment while lacking insurance, inability to pay, or fear of non-citizens being questioned about immigration status.11 The best way to understand the pain is to ask the patient to describe and rate the pain in their own words. Showing concern for the patient’s pain is as important as providing the analgesia itself.12
Young and advanced age, cognitive impairment, comorbidities, and polypharmacy result in challenging presentations during an assessment.13,14 Additionally, feared side effects such as clouded or impaired judgment and disabled capacity are cited as arguments against aggressive pain management. Added precautions of side effects and polypharmacy could account for early oligoanalgesia in these individuals. Specific training focused on treating these groups can eliminate this apprehension.15
Limiting analgesia among patients pending a surgical evaluation may also result delays in pain management. These delays in analgesic administration may not only cloud a patient’s judgment when making decisions on further tests and treatment, it may also hinder the ability of a health care provider to perform a thorough physical examination to identify the underlying pain source.16,17
Negative stereotypes or stigmatization of those in pain may also result in an underestimation of pain presentations. However, genetic polymorphisms in drug metabolism between individual patients can result in significant variability in response to pain medications and could result in a limited response to a standard pain regimen. Drug-seeking behavior should be considered a diagnosis of exclusion.
PAIN ASSESSMENT IN THE ED
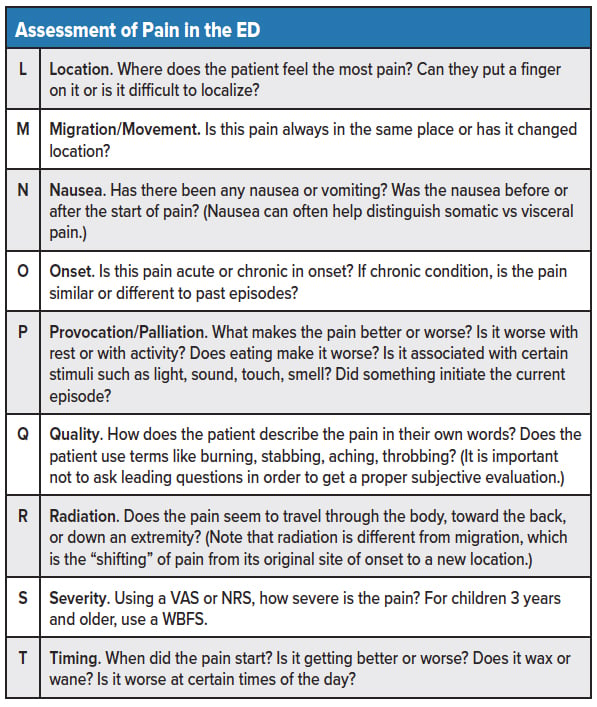
The approach to pain in the emergency room is similar to any other chief complaint. The provider must identify whether the painful condition is acute or chronic, limb or life-threatening, associated with underlying illness, distracting from other injuries, and whether it requires immediate resuscitative attention. Assessments may be challenging with known chronic disease, or pain conditions present an opportunity for early diagnostic anchoring. If a chronic condition exists, assess whether the pain is similar or different from past episodes. If chronic, determine what initiated/exacerbated the current episode and whether anything relieves or worsens the pain.
After conducting a primary assessment of ABCs and effectively ruling out any emergent issues, the provider can proceed with a more detailed history and physical of the pain syndrome (see table).
PAIN CLASSIFICATION
Pain is classified as three main types: Acute, Chronic, and Acute on Chronic.
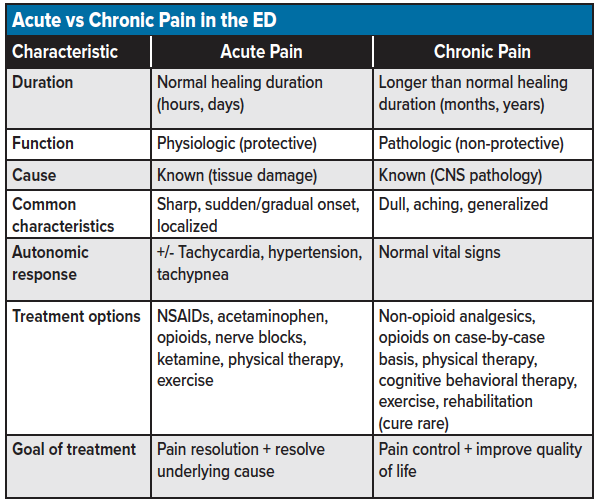
Acute pain is the classic pain associated with a known underlying physiologic cause, such as tissue-derived nociception (perceived or actual tissue injury). Onset can be sudden or gradual, and the duration is typically short. Less than one month (but up to three months) has been used as an arbitrary cutoff and should be considered relative to the disease process (versus sub-acute pain, 3-12 months). Acute pain associated with trauma, fracture, or tissue ischemia is often associated with tachycardia, tachypnea, and hyper-(hypo-) tension. Acute pain typically disappears with the resolution of the underlying cause. Analgesic choices for acute pain focus on the type and severity of pain.
Chronic pain is considered a diseased state in which the normal time of healing for the associated injury has passed.18 Over 30% of the U.S. population experience some form of chronic pain, women more frequently than men.2 The most common cause of chronic pain is back pain.2 Although chronic pain can result from an acute injury, the result is typically pathologic, secondary to an upregulation of pain signaling receptors, resulting in central and peripheral nerves developing a hypersensitivity to stimuli.19 The pain is described as dull or aching; stabbing, a sharp pain is also possible. Chronic pain is typically of unknown duration, extending over months to years. Vital signs are usually stable. Chronic pain may arise from psychological states and typically has no recognizable end-point.18 Risk factors for chronic pain include suboptimally treated acute pain, increasing age, elevated BMI, multiple comorbidities, and female gender.4 The treatment of chronic pain focuses on controlling the pain and improving quality of life, physical therapy, exercise, and rehabilitation involving a multidisciplinary approach.18 Curing chronic pain is rare. As acute pathology can always occur in the presence of a chronic pain condition, chronic pain pathology is a diagnosis of exclusion (see table for a breakdown of acute vs. chronic pain).
Neuropathic pain is a distinct form of chronic pain defined as pain that arises as a direct consequence of a lesion or diseases affecting the somatosensory system.20 Examples include trigeminal neuralgia, postherpetic neuralgia, multiple sclerosis or stroke-related pain, diabetic and HIV-related neuropathy, and post-amputation pain. Neuropathic pain is estimated to affect 7-10% of the population,21 constituting a significant burden to society and the individual quality of life.22 Characteristics of neuropathic pain include burning or “pins and needles” sensation, severe itching or electric shocks, pain in an area of partial or complete sensory loss, increased pain after repetitive stimulation, persistent pain following stimulation discontinuation, pain due to a stimulus that does not usually provoke pain (allodynia), and increased pain from a stimulus that generally provokes pain (hyperalgesia).23,24 It is essential to distinguish neuropathic pain from other forms of chronic pains as the treatment modalities are unique.
Acute on chronic pain is associated with an acute exacerbation of a chronic condition. An example is a sickle cell vaso-occlusive pain crisis in a chronic sickle cell patient. The combination of an acute presentation overlaying a chronic condition can result in extensive variability in duration, characteristics, autonomic response, treatment options, and goals of treatment.
PAIN SCALES
Pain scales are predominantly utilized in analgesic research, where intervention comparisons are required to assess the efficacy and superiority of different study medications.25,26 Although pain scales are recommended in the emergency department, the utility of the scales is limited due to unimodal and quantitative characteristics. It is more prudent to have the patient describe their pain subjectively in their own words. Pain scores are most accurate when reported by the patient and repeated at several time points during treatment to assess the efficacy of the analgesic regimen.
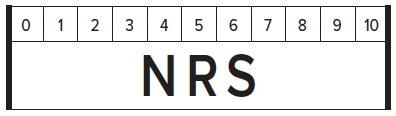
Numerical pain scales may be used to assess the effectiveness of an analgesic regimen among adult patients. Two commonly used pain scales are the Visual Analog Scale (VAS) and the Numerical Rating Scale (NRS) (see image 1). The value on a pain scale is in the representation of pain at a particular point in time based on the patient's personal experiences. The purpose of the reference point at ED arrival is to assess the severity of the patient’s pain and illness and as a starting point for reassessment following the initiation of an analgesic regimen. Early pain assessment in the ED should also include a qualitative evaluation of the patient’s baseline functional status and goals of treatment.
The VAS is a 100 mm linear scale ranging from no pain, 0mm, to worst pain imaginable, 100mm. During the initial evaluation, the patient is asked to rate their pain on the scale, and the distance is measured from left to right in millimeters (0 to 100); this value is used as the baseline pain rating. Follow up VAS scores can be used to assess the efficacy of analgesic treatment. A difference of >13 mm has been validated as the minimal clinically significant difference in pain rating (clinical significance), whereas >30 mm is the minimum acceptable change for acceptable pain improvement (analgesic response).26,27 The VAS is challenging to utilize in a trauma setting and severe pain situations. The VAS has demonstrated utility in contexts of language difficulties and cross-cultural differences where descriptive terms may be misinterpreted in translation.28
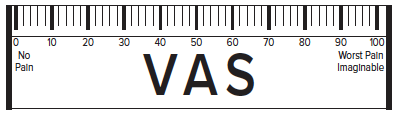
The NRS is an 11-point numerical (non-linear) scale from 0 to 10, 10 being the most severe pain. In contrast to the VAS, the NRS can be done visually or verbally, is more reliable, and easier to use in trauma scenarios.29 The minimum clinically significant difference in pain on an NRS scale is 1.3.6 Research has shown that the NRS and VAS correlate closely with each other and can be used interchangeably.6
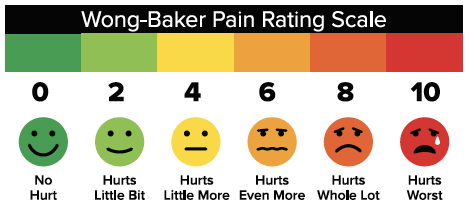
Non-numerical scales are best used in the evaluation of pain among pediatric patients. An example is the Wong-Baker Scale (WBS)30, which provides a visual rating scale used for patients three and older from no hurt, zero, to hurts worst, 10. As opposed to a numerical rating scale used among the adult population, the WBS utilizes a facial expression pain scale which is preferable among the children who lack the ability to describe their pain in detail.31
Rating tools are limited by the patient's ability to convert a noxious stimulation to a numerical representation and are heavily influenced by past pain experiences and the ability to tolerate pain. Ultimately it is the patient’s subjective reporting of pain and its effect on their functionality that will give providers the best understanding of the degree of pain and the analgesic modality required to effectively treat the patient. It is important to note that the ultimate goal of analgesic management is not zero pain, but a reduction that allows a patient to return their daily activities of life. A shared discussion with the patiet prior to treatment initiation will help create a shared understanding and appreciation of this objective.
Summary
The ability to recognize and understand the different pain presentations is an essential skill of any emergency provider. With an expanded understanding of the factors contributing to the undertreatment of pain as well as knowledge on the proper classification and organization of pain characteristics, pain can be quickly identified and addressed in the emergency setting. Pain assessment scales such as the VAS and NRS may be used as adjuncts to assess baseline pain and follow-up analgesic efficacy. However, the assessment of pain in the ED should be based on a need for analgesia to improve – and whenever possible, restore – a patient's functional status. Following the initial recognition and assessment of pain, the provider can now approach the effective treatment of each specific pain presentation.
References
- Merskey H, Bogduk N. Classification of Chronic PainDescriptions of Chronic Pain Syndromes and Definitions of Pain Terms. Task Force on Taxonomy of the International Association for the Study of Pain. 1994; 2nd ed.
- Todd KH, Ducharme J, Choiniere M, et al. Pain in the emergency department: results of the pain and emergency medicine initiative (PEMI) multicenter study. J Pain. 2007;8:460-6.
- National Hospital Ambulatory Medical Care Survey: 2015 Emergency Department Summary Tables www.cdc.gov: US Department of Health and Human Services 2015.
- Gallagher RM. Physician variability in pain management: are the JCAHO standards enough? Pain Med. 2003;4:1-3.
- O’Connor AB, Zwemer FL, Hays DP, Feng C. Outcomes after intravenous opioids in emergency patients: a prospective cohort analysis. Acad Emerg Med. 2009;16:477-87.
- Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med. 2003;10:390-2.
- Curtis L MT. Pain Management in the Emergency Department. EB Medicine. 2006;8.
- Hwang U, Richardson LD, Harris B, Morrison RS. The quality of emergency department pain care for older adult patients. J Am Geriatr Soc. 2010;58:2122-8.
- Mills AM, Shofer FS, Boulis AK, Holena DN, Abbuhl SB. Racial disparity in analgesic treatment for ED patients with abdominal or back pain. Am J Emerg Med. 2011;29:752-6.
- Platts-Mills TF, Hunold KM, Bortsov AV, et al. More educated emergency department patients are less likely to receive opioids for acute pain. Pain. 2012;153:967-73.
- Cunningham PJ. What accounts for differences in the use of hospital emergency departments across US communities? Health Aff (Millwood). 2006;25:w324-36.
- Motov SM, Khan AN. Problems and barriers of pain management in the emergency department: Are we ever going to get better? J Pain Res. 2008;2:5-11.
- Sampson EL, White N, Lord K, et al. Pain, agitation, and behavioural problems in people with dementia admitted to general hospital wards: a longitudinal cohort study. Pain. 2015;156:675-83.
- Sengstaken EA, King SA. The problems of pain and its detection among geriatric nursing home residents. J Am Geriatr Soc. 1993;41:541-4.
- Choo EK, Mazer-Amirshahi M, Juurlink D, Kobner S, Scott K, Lin M. The Prescription Opioid Epidemic: Social Media Responses to the Residents’ Perspective Article. Ann Emerg Med. 2016;67:40-8.
- Post LF, Blustein J, Gordon E, Dubler NN. Pain: ethics, culture, and informed consent to relief. J Law Med Ethics. 1996;24:348-59.
- LoVecchio F, Oster N, Sturmann K, Nelson LS, Flashner S, Finger R. The use of analgesics in patients with acute abdominal pain. J Emerg Med. 1997;15:775-9.
- Grichnik KP, Ferrante FM. The difference between acute and chronic pain. Mt Sinai J Med. 1991;58:217-20.
- Dinakar P, Stillman AM. Pathogenesis of Pain. Semin Pediatr Neurol. 2016;23:201-8.
- Neuropathic Pain. Last accessed Oct 8, 2019/2019.
- van Hecke O, Austin SK, Khan RA, Smith BH, Torrance N. Neuropathic pain in the general population: a systematic review of epidemiological studies. Pain. 2014;155:654-62.
- Smith BH, Torrance N. Epidemiology of neuropathic pain and its impact on quality of life. Curr Pain Headache Rep. 2012;16:191-8.
- Jensen TS, Finnerup NB. Allodynia and hyperalgesia in neuropathic pain: clinical manifestations and mechanisms. Lancet Neurol. 2014;13:924-35.
- Jensen TS, Baron R. Translation of symptoms and signs into mechanisms in neuropathic pain. Pain. 2003;102:1-8.
- Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med. 2001;8:1153-7.
- Gallagher EJ, Liebman M, Bijur PE. Prospective validation of clinically important changes in pain severity measured on a visual analog scale. Ann Emerg Med. 2001;38:633-8.
- Todd KH, Funk KG, Funk JP, Bonacci R. Clinical significance of reported changes in pain severity. Ann Emerg Med. 1996;27:485-9.
- Heins A, Homel P, Safdar B, Todd K. Physician race/ethnicity predicts successful emergency department analgesia. J Pain. 2010;11:692-7.
- Berthier F, Potel G, Leconte P, Touze MD, Baron D. Comparative study of methods of measuring acute pain intensity in an ED. Am J Emerg Med. 1998;16:132-6.
- Gaglani A, Gross T. Pediatric Pain Management. Emerg Med Clin North Am. 2018;36:323-34.
- Miro J, Huguet A. Evaluation of reliability, validity, and preference for a pediatric pain intensity scale: the Catalan version of the faces pain scale--revised. Pain. 2004;111:59-64.