Ch. 12 - Pediatric Pain
Taryn L. Webb, MD | Icahn School of Medicine at Mount Sinai
Jennifer E. Sanders, MD | Icahn School of Medicine at Mount Sinai
Pain is one of the most common presenting emergency department (ED) complaints among pediatric patients, with episodic, acute, or exacerbations of chronic pain, making up about 78% of all emergency department (ED) visits.1 Musculoskeletal injuries, abdominal pain, sore throat, otalgia, and headache are some of the more commonly presenting pain etiologies.
Pain among the youngest patients is often multifactorial and can be especially challenging to assess in pre-verbal children.2 The perception of pain in pediatrics is also involved and entails physiologic, behavioral, psychological, and developmental factors.3 Often, children do not exhibit the typical signs and symptoms of pain, or they may be reacting to family emotions or behavioral cues.2 Given this, a holistic approach to the evaluation and management of a child in pain is required to recognize and treat pain successfully. This approach includes consideration of the child's age and developmental stage, how the child is interacting and reacting with his/her environment, consideration of any particular circumstances such as a terminal illness, and the evaluation of family/caregiver dynamics.2
Unfortunately, research has shown that pediatric pain is frequently undertreated (oligoanalgesia), and this is especially true in the younger populations and those with cognitive impairments. Common causes of oligoanalgesia include an inability to recognize pain (visual and behavioral cues), decreased perception of pain, a lack of awareness of analgesic modalities, incorrect medication dosing, and fear of medication side effects/toxicity.4 In a study by Yackey et al., only 54% of children under four years of age with extremity fractures received analgesia, and of those children, only 21% were given opioids.4 Research has also shown that patients who experience pain early in life demonstrate long-term changes in perception of pain and related behaviors.3,5 Similarly, uncontrolled or severe pain can lead to the development of hyperalgesia later in life, further emphasizing the importance of effective pain management in this age group.1 The purpose of this chapter is to discuss the proper recognition and assessment of pediatric pain (including a discussion on age-specific pain scales), review on pharmacologic and nonpharmacologic analgesia modalities, discuss special population considerations, and review the disposition of patients presenting with pain.
PRINCIPLES OF PEDIATRIC PAIN MANAGEMENT IN THE ED
The guiding principles to pediatric pain management include:
- Recognition of the age-appropriate signs, symptoms, and pain scales used on pediatric patients
- Allowance for self-reporting when possible (involve caregivers when appropriate)
- Prompt analgesic administration following pain recognition
- Early and frequent pain reassessments
RECOGNITION AND ASSESSMENT OF PEDIATRIC PAIN
The initial pain assessment of a pediatric patient involves a discussion with both the child and the parent/caregiver tailored to the patient's age and the clinical context. Whenever possible, the patient's self-report of pain severity is considered the gold standard. However, because the pain in the pediatric population is challenging to assess, several age-specific pain management tools and scales have been created to assist in quantifying the level of pediatric pain (See table 1 for a list of pain scales by age group). These tools are especially crucial for pre-verbal or non-verbal children, who may only demonstrate signs of discomfort or distress such as excessive crying, irritability, poor feeding, position and movement of extremities, sleeplessness, altered facial expression, and vital sign variability.
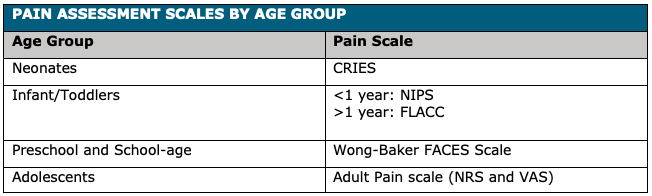
Neonates
Pain recognition among neonates represents a unique challenge, as they do not demonstrate typical pain behaviors. Due to developing nervous systems and an under-developed ability to express pain, providers must focus on physiologic changes and visible behavioral cues such as furrowed brows, eyes squeezed shut, expressionless vertically open mouth, abnormal movement of arms and legs, inability to be consoled, disturbed sleep patterns, and vital sign changes such as tachycardia and tachypnea.
A commonly used scale among neonates to assess pain is the CRIES scale. The CRIES scale is an 11-point pain scale (0 to 10) which utilizes an acronym based on five physiological and behavioral variables shown to be associated with neonatal pain: C--Crying; R--Requiring increased oxygen administration; I—Increasing (abnormal) vital signs; E—Expression (facial); S—Sleeplessness (see Table 2 for a breakdown of the CRIES Pain Scale scoring system). The absolute value of the initial CRIES score should only be used as a baseline assessment. The purpose of the CRIES score (and all other pain scores) is to assess the efficacy of the pharmacologic and nonpharmacologic interventions by trending the score over time.
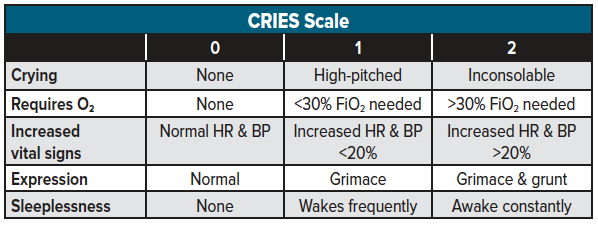
Infants/Toddlers
The pain assessment scales used among infants and toddlers differ for those younger and older than age one year:
- <1 year: Neonatal Infant Pain Scale (NIPS)
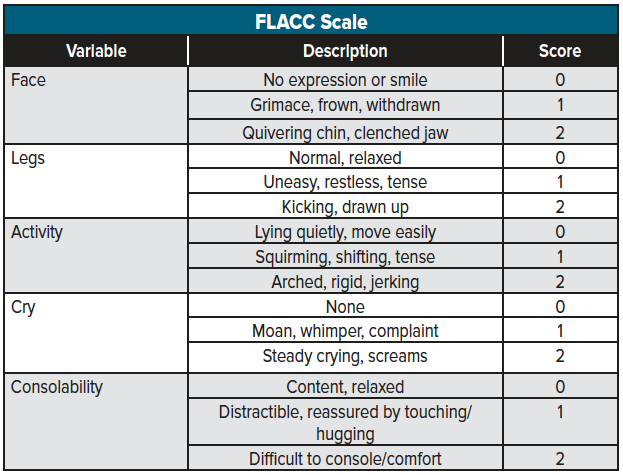
- >1 year: Face, Legs, Activity, Cry, Consolability (FLACC) Scale
The Neonatal Infant Pain Scale (NIPS) is an 8-point pain scale (0 to 7) based on six variables that may be used among both full-term and pre-term infants (See table 3 for a NIPS scoring breakdown). A score of 3-4 indicates mild to moderate pain that may be managed with non-pharmacologic intervention, whereas a score of 5 or more indicates severe pain, which typically requires pharmacologic interventions.
The Face, Legs, Activity, Cry, Consolability (FLACC) scale is an 11-point pain scale (0 to 10) used to assess pain in children > 1-year-old who are unable to communicate their pain accurately and has been validating in the emergency setting 6 (See table 4 for a FLACC scoring breakdown). Similar to the other pain scores, the absolute value should be trended over time to assess the efficacy of the analgesic treatments administered.
Preschool & School-age children
Pain assessment among older, school-aged children with increased language skills becomes easier for providers by allowing direct verbal communication using descriptors. However, providers should be cautious with leading questions as many preschoolers will answer "yes" to all questions and may be easily instructable. Instead, corroborate with the parent/caregiver about changes in behaviors they have noticed (i.e., limping, holding one ear, withdrawn from normal activities, inadequate oral intake). Among verbal children >3 years of age, the Wong-Baker FACES Pain Scale, which utilizes a series of 6 faces increasing in pain severity may be used to facilitate communication and assist in pain assessment (See Figure 1 for a description of the Wong-Baker Pain Rating Scale).
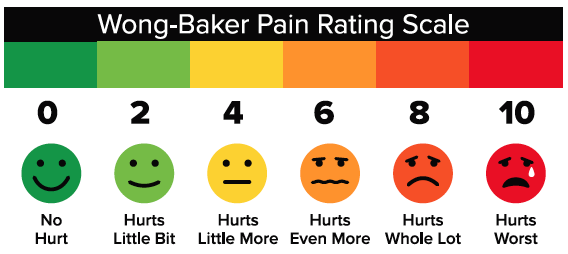
Figure adapted from the Wong-Baker FACES Foundation – www.WongBakerFACES.org
Adolescents
Assessing pain among adolescents varies based on the level of maturity and intellectual development. Although the Wong-Baker FACES Pain Rating Scale may be considered, many adolescents (particularly teenage patients) may effectively rate pain using adult rating scales such as the Numerical Rating Scale(NRS) and the Visual Analogue Scale (VAS) (See chapter 1 for a description of these adult pain rating scales).
Note that pain expressions and numerical reporting can vary from child to child. Regardless of the pain scale used, the original score should serve as guidance in assessing the efficacy of continuing analgesic management with frequent reassessments conducted using the same scale and emphasis being placed on the change in the score over time rather than the absolute value.
NON-PHARMACOLOGIC ANALGESIC ALTERNATIVES
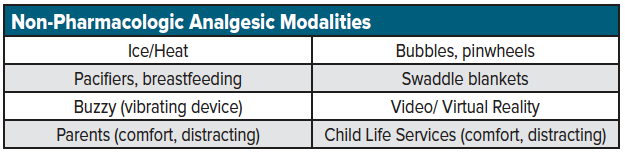
Non-pharmacologic agents should be considered the first line for pediatric pain control in the ED. These agents are typically the safest and may act as an effective bridge to pharmacologic treatment options. Non-pharmacologic alternatives can be broken down into two categories: physical comfort measures and distracting activities. Whereas physical comfort measures are most effective in neonates and younger children, distraction is typically employed in older children and adolescents. Regardless of age, consider utilizing Child Life Services whenever possible to assist in comfort and distraction measures (See table for a list of commonly used non-pharmacologic options).
Key Considerations When Initiating Pain Management
Neonates/infants (0-12 months)
- Engage and comfort the parent, encourage them to hold and comfort the patient
- Utilize soothing sensory measures (gentle touch), speak softly
- Use comfort techniques: pacifier, swaddle
Toddlers to Preschool (1-5 years)
- Engage and comfort the parent, encourage them to hold and comfort the patient
- Utilize soothing sensory measures (gentle touch), speak softly
- Communicate in simple, direct language: describe what they will see, hear, and feel; give calm, firm directions
- Demonstrate procedures with a doll/toy before the patient administration/procedure
- Offer choices when appropriate
- Use distraction techniques: storytelling, bright/flashy toys, BUZZY, bubbles, pinwheels, Child Life Services
School-age (6-12 years)
- Communicate in simple, direct language explain the procedure and reason why
- Allow them to ask questions, involve when possible/appropriate
- Use distraction techniques: electronic games, videos, guided imagery, participation
- Consider comfort measures such as positioning, splint/ACE wrap, ice or heat packs
Adolescent (13+)
- Communicate in simple, direct language to explain the procedure, and the reason why; detail and encourage questioning; be flexible
- Use distraction techniques: electronic games, videos, guided imagery, participation, relaxation/meditation, music
- Consider comfort measures such as positioning, splint/ACE wrap, ice or heat packs
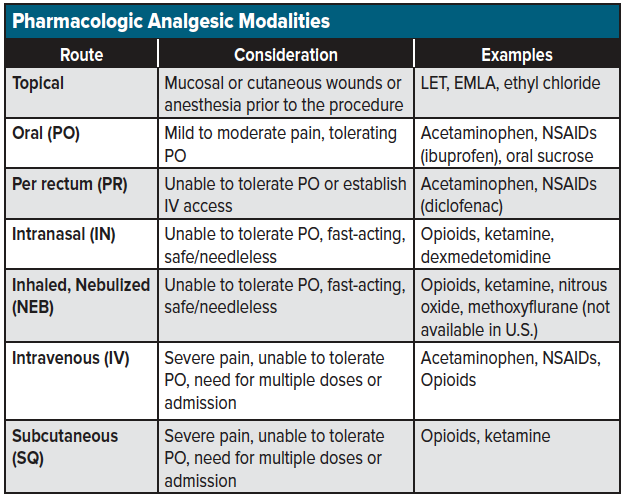
PHARMACOLOGIC ANALGESIC MODALITIES
Although non-pharmacologic options are considered first-line among the pediatric population, patients with moderate and severe pain often require pharmacologic treatment options for adequate pain control. It's essential to start with the least invasive routes and safest medications - oral, per rectum, intranasal, inhaled/nebulized, topical – and progress as needed to parenteral options for refractory pain (See table for a list of analgesic options by route). Be sure to speak with the child's parents about drug indication, treatment goals, and anticipation of improvement.
Escalation of Pharmacologic Agents
Pediatric pain management follows a treatment hierarchy depending on the severity of the pain ranging from mild, moderate, to severe. However, regardless of the pain intensity, combination therapy with non-pharmacologic, non-opioid, and opioid analgesic modalities should be implemented.
For mild pain, oral formulations such as acetaminophen, nonsteroidal anti-inflammatory drugs (Ibuprofen, naproxen), and sucrose (infants) are considered the first line. Acetaminophen is a first-line oral agent administered at a dose of 10-15 mg/kg every 4-6 hours (PR, 10 to 20 mg/kg).1 Oral NSAIDs are also the first-line regimen for pediatric patients >3 months, >5kg, and adequate hydration. Note, renal function is still impaired in the first months of life, and renal elimination processes (glomerular filtration and active tubular secretion) do not reach adult maturity until 6–12 months 7. Commonly used oral NSAIDs include ibuprofen 10mg/kg every 6-8 hours and naproxen 5 mg/kg every 8-12 hours (max 15 mg/kg/day). For both oral acetaminophen and NSAIDs confirm weight-based dosing as well as any pre-hospital administration to avoid supratherapeutic dosing.
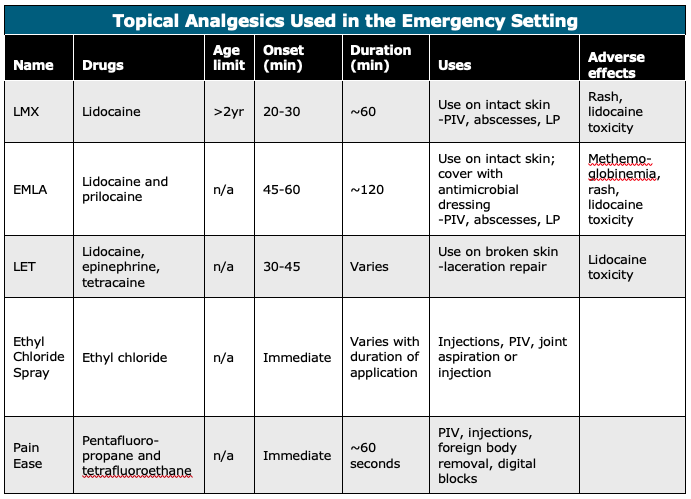
Topical Analgesics
Topical analgesics can also be used for mild to moderate pain as a localized analgesic that limits total-body quantities delivered and systemic distribution (See table for a list of commonly used topical analgesics used among pediatric patients).8,9 Topical analgesics can be utilized for venipunctures, laceration repairs, lumbar punctures, and any other invasive procedure. Common topical formulations include EMLA (Lidocaine + Prilocaine), LET (Lidocaine-Epinephrine-Tetracaine), and ethyl chloride (aka, vapo-coolant). EMLA comes in a cream formulation and requires 45-60 min application prior to onset. LET comes in a gel formulation and requires 30-45 min application prior to onset. Both may be applied to either intact skin or open wounds. Ethyl chloride (vapo-coolant) is an analgesic spray with fast onset and short duration optimal for venipunctures.10
For moderate and severe pain, unresponsive to oral formulations, intranasal, inhaled, and intravenous options may also be considered.
Intranasal (IN) analgesic delivery is a safe, simple, and effective method of analgesia administration that bypasses oral absorption and first-pass metabolism with onset comparable to IV administration. 11 Common IN analgesics include ketamine (1 mg/kg every 1-2 hours), fentanyl (1-2 mcg/kg every 1-2 hours), and hydromorphone (2-5 mg every 4-6 hours). Optimal IN delivery requires both nostrils to maximize the absorption surface area. Unlike IV, no site sterilization is required with IN administration. Typical volumes range from 0.3–0.5 cc and should not exceed 1.0 cc to avoid runoff before absorption.11,12 High-concentration formulations are chosen to minimize the volume and reduce this runoff.13 Though topical administration is feasible, mucosal atomizer devices (MAD) are preferred to optimize distribution. Several studies have assessed the efficacy of IN analgesia for acute musculoskeletal pain among pediatric patients using fentanyl and ketamine, with both showing relative equal effectiveness for short-term pain relief.14,15
Inhaled analgesics include opioids, ketamine, and nitrous oxide. Inhaled nitrous oxide (NO) may be utilized in a 50/50 NO/oxygen concentration among adolescent patients with moderate to severe pain. 16,17 NO has demonstrated analgesic efficacy when used for musculoskeletal fractures/reductions.18 laceration repairs,19 abscess drainage, foreign body removal, urinary catheterization, wound examination, and joint aspiration.20,21
Intravenous analgesia options include NSAIDs (ketorolac), acetaminophen, opioids, and ketamine. The most commonly used intravenous NSAID is ketorolac (0.5 mg/kg every 6-8 hours). Though opioid utilization should be minimized among the pediatric population, severe pain, sickle cell pain, cancer-related pain, and pain refractory to alternatives may require a trial of opioids. Common opioids use among pediatric patients include morphine (0.05-0.1 mg/kg q2-4hrs), hydromorphone (0.01 mg/kg every 4-6 hours), and fentanyl (1 mcg/kg every 1-2 hours).22
Regional anesthesia (peripheral nerve blocks) is also an effective analgesic modality for moderate to severe pain presentations among the pediatric population. Similar to adults, nerve blocks may effectively treat laceration repairs, musculoskeletal fractures/reductions, and foreign body removal. Common anesthetics include lidocaine, bupivacaine, and prilocaine (see the chapter on nerve blocks for further discussion).
SPECIAL POPULATIONS/CONSIDERATIONS
Chronic medical problems such as sickle cell crises, juvenile idiopathic arthritis (JIA), and cancer-related pain often require special analgesic consideration. These patients may have previous unpleasant experiences and amplified anxiety/perception of pain. Chronic pain typically requires a multimodal approach that incorporates the patient's home analgesic regimens (see the chapter on chronic pain for further discussion). For acute exacerbations of these chronic ailments, inquire about previous pain management regimens, and baseline analgesic utilization. Titration is best accomplished through intravenous administration with patient-controlled analgesia (PCA) pumps serving as a common tool used for admitted patients.1,23
Cognitive impairment secondary to genetic/metabolic conditions, neurologic disability(eg, cerebral palsy, autism spectrum disorder, Down Syndrome) presents the difficulty of explaining or expressing pain. These patients may also have atypical expressions of pain, such as smiling or laughing, stiffening, or being uncooperative. The "freezing phenomenon" may also occur, which has been described as abrupt pauses in the patient's activity and facial movements. When managing pain in patients with cognitive impairment, focus on physiologic changes such as unexplained pallor, diaphoresis, breath-holding, and shrill vocalizations. Consider using the FLACC scale for pain assessment regardless of age. Additionally, children with autism spectrum disorders (ASD) may recover more slowly from noxious stimuli than other pediatric patients.1 Patients with Down Syndrome typically show delayed expression of pain and have difficulty with localizing their symptoms.1 Be sure to consider the pharmacokinetic and pharmacodynamic variations among patients with metabolic disorders and syndromes who may have variable metabolism and excretion.
Palliative Care. Pediatric patients under palliative care should have their pain managed under a multidisciplinary approach with consideration of their underlying analgesic pain plan. When treating these patients, speak with their family and care team to focus on treatments that will be beneficial and productive to their pain management quality of life goals. Consider the fact that these patients may encounter complications of chronic opioid treatment such as nausea/vomiting, constipation, and urinary retention, which may be the etiology of their pain presentation.
PEDIATRIC PAIN DISPOSITION
The majority of children who require analgesia can be safely discharged home if the pain is well controlled, and the child can walk unsupported and tolerate fluids. If outpatient analgesia is required, most children will do well with acetaminophen or ibuprofen for pain control, even for fractures and post-op pain control. Occasionally, the patient will need a short course of oral opioids for pain control. Consider a short, 2-3 day course of morphine sulfate immediate release (MSIR) with an emphasis on discontinuing and flushing medications once pain resolves. Those patients requiring multiple IV doses of medication should be admitted to an inpatient or observation setting for further pain management.
PEDIATRIC PAIN SUMMARY
Children of all ages are responsive to painful stimuli, and pain and injury in early life can lead to long-term adverse consequences and pain hypersensitivity if undertreated. Treat pain promptly and reassess frequently using the baseline pain scale score for assessment of analgesic efficacy. Non-pharmacologic interventions should be combined with pharmacologic interventions as a multimodal approach to address pediatric pain and always consider a stepwise approach using oral, topical, nebulized, intranasal, and intravenous routes depending on the severity of presenting pain. Younger infants and those with cognitive impairment may express pain in unique and unexpected ways; consider physiologic variables in non-verbal patients, but when possible, allow the child to speak for themselves.
References
- Krauss BS, Calligaris L, Green SM, Barbi E. Current concepts in management of pain in children in the emergency department. Lancet. 2016;387(10013):83-92.
- Horezco T. Acute Pain in Children. Pain & Procedural Sedation in Acute Care https://painandpsa.org/peds/. Accessed 10/4, 2019.
- Srouji R, Ratnapalan S, Schneeweiss S. Pain in children: assessment and nonpharmacological management. Int J Pediatr. 2010;2010.
- Yackey KJ, Rominger AH. Are We Adequately Treating Pain in Children Who Present to US Emergency Departments?: Factors That Contribute to Pain Treatment in Pediatric Patients. Pediatr Emerg Care. 2018;34(1):42-46.
- Taddio A, Katz J, Ilersich AL, Koren G. Effect of neonatal circumcision on pain response during subsequent routine vaccination. Lancet. 1997;349(9052):599-603.
- Kochman A, Howell J, Sheridan M, et al. Reliability of the Faces, Legs, Activity, Cry, and Consolability Scale in Assessing Acute Pain in the Pediatric Emergency Department. Pediatr Emerg Care. 2017;33(1):14-17.
- Fernandez E, Perez R, Hernandez A, Tejada P, Arteta M, Ramos JT. Factors and Mechanisms for Pharmacokinetic Differences between Pediatric Population and Adults. Pharmaceutics. 2011;3(1):53-72.
- Leppert W, Malec-Milewska M, Zajaczkowska R, Wordliczek J. Transdermal and Topical Drug Administration in the Treatment of Pain. Molecules. 2018;23(3).
- McCarberg B, D'Arcy Y. Options in topical therapies in the management of patients with acute pain. Postgrad Med. 2013;125(4 Suppl 1):19-24.
- Griffith RJ, Jordan V, Herd D, Reed PW, Dalziel SR. Vapocoolants (cold spray) for pain treatment during intravenous cannulation. Cochrane Database Syst Rev. 2016;4:CD009484.
- Kalviainen R. Intranasal therapies for acute seizures. Epilepsy Behav. 2015;49:303-306.
- Tsze DS, Ieni M, Fenster DB, et al. Optimal Volume of Administration of Intranasal Midazolam in Children: A Randomized Clinical Trial. Ann Emerg Med. 2017;69(5):600-609.
- Bailey AM, Baum RA, Horn K, et al. Review of Intranasally Administered Medications for Use in the Emergency Department. J Emerg Med. 2017;53(1):38-48.
- Graudins A, Meek R, Egerton-Warburton D, Oakley E, Seith R. The PICHFORK (Pain in Children Fentanyl or Ketamine) trial: a randomized controlled trial comparing intranasal ketamine and fentanyl for the relief of moderate to severe pain in children with limb injuries. Ann Emerg Med. 2015;65(3):248-254 e241.
- Reynolds SL, Bryant KK, Studnek JR, et al. Randomized Controlled Feasibility Trial of Intranasal Ketamine Compared to Intranasal Fentanyl for Analgesia in Children with Suspected Extremity Fractures. Acad Emerg Med. 2017;24(12):1430-1440.
- American Society of Anesthesiologists Task Force on S, Analgesia by N-A. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;96(4):1004-1017.
- Reinoso-Barbero F, Pascual-Pascual SI, de Lucas R, et al. Equimolar nitrous oxide/oxygen versus placebo for procedural pain in children: a randomized trial. Pediatrics. 2011;127(6):e1464-1470.
- Luhmann JD, Schootman M, Luhmann SJ, Kennedy RM. A randomized comparison of nitrous oxide plus hematoma block versus ketamine plus midazolam for emergency department forearm fracture reduction in children. Pediatrics. 2006;118(4):e1078-1086.
- Bar-Meir E, Zaslansky R, Regev E, Keidan I, Orenstein A, Winkler E. Nitrous oxide administered by the plastic surgeon for repair of facial lacerations in children in the emergency room. Plast Reconstr Surg. 2006;117(5):1571-1575.
- Tobias JD. Applications of nitrous oxide for procedural sedation in the pediatric population. Pediatr Emerg Care. 2013;29(2):245-265.
- Huang C, Johnson N. Nitrous Oxide, From the Operating Room to the Emergency Department. Curr Emerg Hosp Med Rep. 2016;4:11-18.
- Berde CB, Sethna NF. Analgesics for the treatment of pain in children. N Engl J Med. 2002;347(14):1094-1103.
- Zernikow B, Schiessl C, Wamsler C, et al. [Practical pain control in pediatric oncology. Recommendations of the German Society of Pediatric Oncology and Hematology, the German Association for the Study of Pain, the German Society of Palliative Care, and the Vodafone Institute of Children's Pain Therapy and Palliative Care]. Schmerz. 2006;20(1):24-39.