Ch. 5 - Renal Colic Pain
Sergey M. Motov, MD, FAAEM | Maimonides Medical Center
John P. Marshall, MD, MBA, FACEP | Maimonides Medical Center
Renal colic represents one of the worst painful conditions, affecting approximately 12% of the population.1 Renal colic causes 1.2 million people to seek care each year and accounts for 1% of all emergency department (ED) visits and 1% of all hospital admissions. In 50% of patients with a history of kidney stones, recurrence rates approach nearly 50% after ten years.2
The pain of renal colic origin is multifactorial. Obstruction of urinary flow secondary to stone passage results in an increased intrarenal and intra-ureteral pressure as well as prostaglandin-mediated ureteral spasm.1,3 The pain is usually acute in onset, severe in intensity, and frequently associated with nausea, vomiting, and hematuria. Therefore, timely and effective analgesia for patients presenting to the ED with the pain of renal colic origin is of utmost importance for ED doctors.
This chapter will focus on reviewing therapeutic options available to ED physicians that include traditional and most commonly used classes of analgesics such as non-steroidal anti-inflammatory drugs (NSAIDs) and opioids as well as more controversial and not yet widely accepted analgesic options that include intravenous acetaminophen (APAP), intravenous lidocaine, and intravenous ketamine.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs (parenteral ketorolac and oral ibuprofen in the U.S., parenteral diclofenac in the Middle East, and Europe) are mainstay therapies for patients with renal colic. NSAIDs relieve renal colic pain by inhibiting prostaglandin synthesis, thus preventing afferent arterial vasodilation and reducing ureteral edema, inflammation, and muscular hyperactivity.1,3,4 Oral (PO), rectal (PR), and intramuscular (IM) routes are associated with delayed onset of analgesia, but intravenously (IV) administered ketorolac provides rapid and effective analgesia (comparable with opioids).5 Disadvantages of NSAIDs administration in patients suffering from renal colic include lack of titratability, adverse effects including nausea, vomiting, feeling of heat or pressure in the chest, fatigue, and lethargy. Furthermore, NSAIDs are contraindicated in patients with severe congestive heart failure, renal insufficiency, and acute peptic ulcer disease.4 It is important to emphasize that ketorolac administration via intramuscular route for patients with renal colic is associated with unnecessary pain upon injection, the prolonged onset of analgesia (30-60 min), and lack of an analgesic response in about 25% of patients.5,6
In general, all NSAIDs are similar in their ability to relieve pain associated with renal colic. Based on the two-decade-old research, ibuprofen 800 mg PO, ketorolac 30 mg IV or 60 mg IM, diclofenac 50-75 mg IM, and naproxen 500 mg PO are a few of the commonly used NSAIDs. A study comparing intramuscular ketorolac (30 mg) and diclofenac (75 mg) demonstrated no difference between the two groups with respect to analgesic response, rates of rescue analgesia, or side effects.7 However, NSAIDs as a class provide superior pain relief for patients with acute pain due to nephrolithiasis in comparison to non-opioid and opioid analgesics. A recent Cochrane review assessing the benefits and harms of different NSAIDs and non-opioid analgesics in the treatment of adult patients with acute renal colic demonstrated analgesic superiority of NSAIDs when compared with placebo and various antispasmodics.8 Intravenous ketorolac administered at 30 mg dose was found to have a better analgesic response than 100 mg intravenous lidocaine in relieving renal colic pain up to 60 minutes.9
Similarly, intramuscular ketorolac administered at doses of 30 and 60 mg to patients with renal colic demonstrated analgesic superiority, more significant safety profile, a reduced need for rescue analgesia, and faster discharge from the ED in comparison to intramuscular meperidine.10,11 Further, systematic reviews comparing analgesic efficacy and side effect profile of NSAIDs, opioids, and paracetamol (acetaminophen) showed a greater analgesic response, better safety profile (less vomiting) and a reduced need for rescue analgesia in the NSAIDs group.3,12 Lastly, a randomized trial comparing IM diclofenac with IV morphine and IV paracetamol demonstrated a slightly higher percentage of patients achieving > 50 % pain relief at 30 min in the diclofenac group with a significantly lower rate of side effects.13
NSAIDs administered via parenteral and enteral routes follow the concept of "analgesic ceiling" - a pharmacological phenomenon that implies that there is a dosing threshold above which any further increase in a dose would not result in additive analgesia (better pain relief). This concept has not been honored in the above mentioned studies evaluating the use of parenteral ketorolac for renal colic whose analgesic ceiling dose is 10 mg.14 Furthermore, to prove this phenomenon in the ED, a recent randomized trial that compared analgesic efficacy of intravenous ketorolac at three single-dose regimens (10 mg, 15 mg, and 30 mg) for treating acute pain in the ED (including patients with renal colic) demonstrated similar pain relief between three doses up to 120 minutes post-ketorolac administration.15 Thus, the dosing regimen of ketorolac for treating patients with renal colic in the ED should be 10 mg per dose (15 mg due to ease of administering 0.5 mL).
In situations where patients are unable to tolerate oral analgesics or and intravenous access is unobtainable, a rectal formulary of diclofenac or indomethacin while not widely used in the U.S., can be used to control renal colic pain. Rectally-administered diclofenac, in comparison to parenteral meperidine demonstrated better and longer lasting analgesia, less side effects and greater patients and staff satisfaction.13,16 A combination of rectal diclofenac and intranasal desmopressin resulted in greater analgesics efficacy and a reduced need for rescue analgesia than rectal diclofenac alone.17 Rectally administered indomethacin, however, provided less rapid analgesia at 20 minutes compared to rectal morphine.18
OPIOIDS
Opioids have a long history of being one of the most frequently used analgesics for patients with renal colic. Their analgesic effects occur primarily through mu-opioid receptor-mediated blockade of neurotransmitter release and pain transmission. Pure mu-opioid receptors agonists are titratable, inexpensive and devoid of an analgesic ceiling.19 Administration of parenteral opioids in the ED may lead to the development of nausea, vomiting, sedation, dizziness, and in some cases, to respiratory depression and hypotension.20 However, with proper dosing and titration, opioids are effective in alleviating pain in ED patients with renal colic. Earlier data on opioid use for renal colic demonstrated good analgesic efficacy of IM-administered meperidine (75-150 mg) and tramadol (100 mg).21,22 However, rates of severe respiratory depression, euphoria, neurotoxicity, and potential for severe drug interaction and developing dependence outweighed the benefits of using these opioids.23,24
Currently, morphine and hydromorphone are the most commonly used opioids for managing renal colic in the ED. Morphine 10 mg IV has demonstrated similar analgesic efficacy to IV meperidine (100 mg) but with significantly reduced rates of side effects.25 Similarly, hydromorphone 1 mg IV for acute renal colic demonstrated increased pain relief, reduced need for rescue analgesia, and fewer hospital admissions in comparison to IV meperidine ( 50 mg).26 However, when hydromorphone is administered in equianalgesic dosing regimen as morphine, it does not provide superior analgesic efficacy, though it does result in higher rates of respiratory depression and euphoria.27 Consider morphine as a first-line agent for renal colic pain refractory to NSAIDs with hydromorphone reserved for patients with pain refractory to NSAIDs and multiple doses of morphine.
The synergy of combining NSAIDs (ketorolac) with opioids (morphine) has the potential to provide superior analgesia with reduced doses of each agent and to result in a lesser degree of side effects. As an example, when morphine (5 mg x 2 doses IV) was combined with ketorolac (15 mg x 2 doses IV), analgesics efficacy, rates of rescue analgesia and side effects profile of the combined regimen were superior to either medication alone in adult patients presenting to the ED with acute renal colic.28 The attempt to replicate these results, however, failed in another randomized trial where analgesic efficacy of a combination group was found to be similar to the ketorolac group and the morphine group with slightly lower rates of rescue analgesia at 40 minutes.29
In situations where venous access cannot be established in a timely fashion, intranasal (IN) and nebulized (NEB) routes of administration might be beneficial. However, the current data on non-invasive opioid administration for patients with renal colic is limited to a single observational study of 23 patients receiving fentanyl 1.5 mcg/kg IN (average dose of 106 mcg) where it was shown to result in an approximate 50% reduction in pain at 5 minutes post-administration.30
ACETAMINOPHEN (APAP, PARACETAMOL)
Acetaminophen (APAP, paracetamol) is a p-aminophenol derivative with weak inhibitory activity of COX (COX-1, COX-2, and COX-3) isoenzymes, which translates into modest analgesic effects. This inhibitory activity blocks prostaglandin-mediated ureteral spasms resulting in analgesic relief in patients with renal colic.31 As a weak analgesic, acetaminophen is frequently combined with opioid and non-opioid agents to control moderate-to-severe pain. Acetaminophen can be administered orally or rectally, and since the FDA approval of intravenous form (Ofirmev) in 2010, there has been a growing interest in evaluating analgesic efficacy of IV administration for patients with renal colic. Multiple studies comparing IV APAP (1 g administered over 15 min) to IV morphine (0.1 mg/kg bolus) have demonstrated either comparable31-33 or superior34 analgesia at 30 minutes with significantly fewer side effects (primarily nausea and vomiting) in the IV acetaminophen group. However, the analgesic advantage of IV APAP over opioids for managing the pain of renal colic is outweighed by the lack of titratability and concern for dosing errors. Furthermore, in the U.S., there is up to a 300-fold cost differential between oral and rectal formulations of acetaminophen compared to IV formulations, which is likely not justified by any marginal improvement in pain relief.35 IV APAP may be advantageous among patients who are unable to tolerate opioids or NSAIDs, or the patient is restricted from oral medication administration.
LIDOCAINE
Lidocaine is the voltage-dependent sodium channel blocking (reversibly) agent that reduces transmission of pain signals in sensory pathways and inhibits ectopic discharges from injured nerves.36 The mechanism by which IV lidocaine relieves pain in patients with renal colic involves a change in sympathetic smooth muscle tone towards ureteral relaxation by reducing the transmission of afferent sensory pathways.37
In situations where opioids or NSAIDs are contraindicated, or their use is associated with undesirable adverse effects, IV lidocaine (preservative-free) may be considered as an alternative. When lidocaine is administered at 1–1.5 mg/kg dose over 10-15 min, it causes minimal side effects (dizziness, tinnitus, periorbital and perioral numbness) that are transient and rapidly reversible.38 Two case series describing the use of IV lidocaine (1.5 mg/kg) for patients with renal colic in the ED showed a nearly 80% reduction in pain score at discharge.37,38
A randomized trial comparing the analgesic efficacy and safety of IV lidocaine and IV morphine demonstrated a significant pain reduction (NRS reduction > 2 points) in 90% of patients in the lidocaine group versus 70% of the patients in morphine group.39 Furthermore, the administration of IV lidocaine (1.5 mg /kg) as an adjunct to IV morphine (0.1 mg/kg) resulted in a faster onset of analgesia and greater reduction in nausea and vomiting in comparison to intravenous morphine alone.40
Recently, however, a randomized trial comparing the analgesic efficacy of the combination of IV lidocaine and ketorolac to each analgesic alone failed to demonstrate analgesic superiority of the combo therapy over ketorolac alone and resulted in higher rates of adverse side effects than ketorolac alone.9 Additionally, lidocaine administered as a single agent showed inferior pain relief to ketorolac, with much higher rates of adverse effects. 9 Although promising, IV lidocaine will need to be studied in larger populations with a broader age range and with underlying cardiac disease before it can be recommended for routine use in the ED.41
KETAMINE
Ketamine's role as a safe and effective analgesic modality for treating a variety of acute painful conditions in the ED has been continuously expanding. Ketamine is a non-competitive N-methyl-D-aspartate (NMDA) and glutamate receptor antagonist that reduces pain, opioid tolerance, and opioid-induced hyperalgesia.42 Ketamine given intravenously in low sub-dissociative, analgesic doses (0.1–0.3 mg/kg over 15 minutes) provides adequate analgesia with minimal effects on hemodynamics, cognition or consciousness.43
Several studies (all conducted outside of the U.S.) have investigated the analgesic efficacy of IV ketamine for the analgesic management of renal colic. A randomized trial comparing pain relief of IV ketamine (0.15 mg/kg) given as an adjunct to IV morphine (0.1 mg/kg) demonstrated superior analgesic response at 10-minutes and 30-minutes post-medication administration in comparison to IV morphine alone.44 Similarly, research has shown that the addition of IV ketamine (0.2 mg/kg) to IV morphine (0.1 mg/kg) resulted in a more significant reduction of pain, nausea, and vomiting in comparison to morphine (0.1 mg/kg) alone but was associated with a higher frequency of dizziness.45
Additionally, intranasal ketamine (1 mg/kg) has been found to provide similar analgesic relief compared to IV morphine (0.1 mg/kg) when measured up to 30 minutes in ED patients with renal colic46 but failed to provide comparable analgesia to IN fentanyl (1 mcg/kg) and resulted in higher rates of adverse effects.47 It is important to emphasize that the above mentioned studies despite their prospective, randomized design had numerous limitations and biases that limited their generalizability. Further research is needed to assess the safety and efficacy of intranasal ketamine in treating acute renal colic in ED patients.
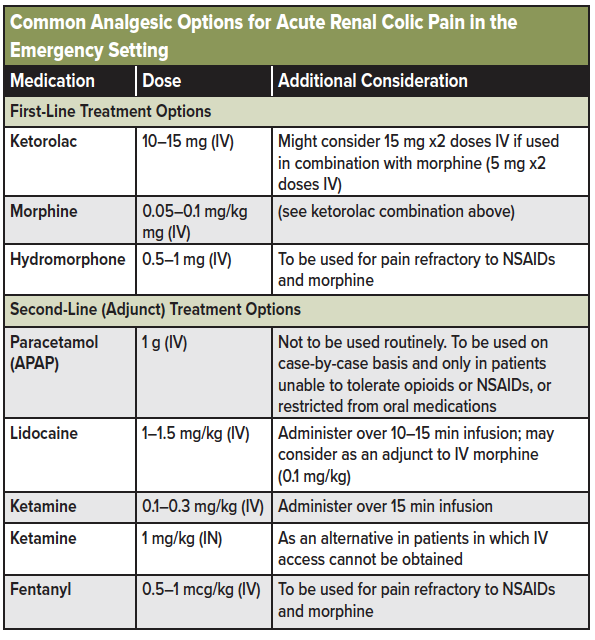
See table 1 below for a list of analgesic options available for renal colic pain in the emergency setting.
DISPOSITION RECOMMENDATIONS
For the patients who show continued pain in the ED setting, an ultrasound or CT-abdomen and pelvis may be warranted to assess for stone size and hydronephrosis.48 Remember, the absence of hematuria does not exclude stones and may be associated with more severe obstructive uropathy.49 Patients with unremitting pain or those unable to tolerate PO will require admission for further management. However, the vast majority of patients will be discharged safely following the above analgesic regimen. Approximately 80% of renal stones < 4 mm pass spontaneously within four weeks and will benefit from outpatient management.50 Only 1 in 8 patients presenting to the ED with renal colic undergo urologic intervention within two months of ED visit, and only 1 in 20 return to the ED within seven days of treatment, indicating that the majority of patients will benefit from outpatient management.51 Consider a short, 3-5-day course of NSAIDs (diclofenac, ibuprofen, naproxen) and urology follow-up for patients stable for discharge. A trial of tamsulosin (0.2–0.4 mg) may be beneficial, particularly in patients with stones > 5–6 mm.52
CONCLUSION
Rapid and effective analgesia is one of the most critical aspect of managing patients with renal colic in the ED. Based on available evidence, NSAIDs are the first-line agents in alleviating the pain of renal colic, with opioids being used as a second-line agent (either as an adjunct to NSAIDs or as a rescue). Opioids should be considered the analgesics of choice when NSAIDs are contraindicated. An appreciation for the undesirable and potentially dangerous side effects of NSAIDs and opioids may require broadening the analgesic armamentarium of ED clinicians by considering alternative classes (and routes of administration) of analgesic medications, including lidocaine and ketamine, and intranasal opioids ( fentanyl). However, in order to utilize these alternatives safely and effectively and to recommend them for broader use, more robust research is needed.
References
- Golzari, S.E., et al., Therapeutic approaches for renal colic in the emergency department: a review article. Anesth Pain Med, 2014. 4(1): p. e16222.
- Talati, J, Tiselius, H.-G, Albala, D.M, YE, Z. Urolithiasis: Basic Science and Clinical Practice. Springer Science & Business Media, Dec 22, 2012.
- Holdgate, A. and T. Pollock, Systematic review of the relative efficacy of non-steroidal anti-inflammatory drugs and opioids in the treatment of acute renal colic. BMJ, 2004. 328(7453): p. 1401.
- Davenport, K. and E. Waine, The Role of Non-Steroidal Anti-Inflammatory Drugs in Renal Colic. Pharmaceuticals (Basel), 2010. 3(5): p. 1304-1310.
- Catapano, M.S., The analgesic efficacy of ketorolac for acute pain. J Emerg Med, 1996. 14(1): p. 67-75.
- Motov, S., et al., Comparison of Intravenous Ketorolac at Three Single-Dose Regimens for Treating Acute Pain in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med, 2017. 70(2): p. 177-184.
- Cohen, E., et al., Comparison of ketorolac and diclofenac in the treatment of renal colic. Eur J Clin Pharmacol, 1998. 54(6): p. 455-8.
- Afshar, K., et al., Nonsteroidal anti-inflammatory drugs (NSAIDs) and non-opioids for acute renal colic. Cochrane Database Syst Rev, 2015(6): p. CD006027.
- Motov, S., et al., Comparison of intravenous lidocaine/ketorolac combination to either analgesic alone for suspected renal colic pain in the ED. Am J Emerg Med, 2019.
- Sandhu, D.P., et al., A comparison of intramuscular ketorolac and pethidine in the alleviation of renal colic. Br J Urol, 1994. 74(6): p. 690-3.
- Larkin, G.L., et al., Efficacy of ketorolac tromethamine versus meperidine in the ED treatment of acute renal colic. Am J Emerg Med, 1999. 17(1): p. 6-10.
- Pathan, S.A., B. Mitra, and P.A. Cameron, A Systematic Review and Meta-analysis Comparing the Efficacy of Nonsteroidal Anti-inflammatory Drugs, Opioids, and Paracetamol in the Treatment of Acute Renal Colic. Eur Urol, 2018. 73(4): p. 583-595.
- Pathan, S.A., et al., Delivering safe and effective analgesia for management of renal colic in the emergency department: a double-blind, multigroup, randomised controlled trial. Lancet, 2016. 387(10032): p. 1999-2007.
- NSAIDs part 2: The Ceiling Effect. https://socmob.org/2013/02/nsaids-part-2-the-ceiling- effect/ ( accessed on 7/18/2020)
- Motov S, Yasavolian M, Likourezos A, Pushkar I, et al. Comparison of Intravenous Ketorolac at Three Single-Dose Regimens for Treating Acute Pain in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med. 2017 Aug; 70 (2):177-184.
- Thompson, J.F., et al., Rectal diclofenac compared with pethidine injection in acute renal colic. BMJ, 1989. 299(6708): p. 1140-1.
- Roshani, A., et al., Assessment of clinical efficacy of intranasal desmopressin spray and diclofenac sodium suppository in treatment of renal colic versus diclofenac sodium alone. Urology, 2010. 75(3): p. 540-2.
- Zamanian, F., et al., Morphine Suppository versus Indomethacin Suppository in the Management of Renal Colic: Randomized Clinical Trial. Pain Res Treat, 2016. 2016: p. 4981585.
- Rowbotham DJ, Serrano-Gomez A, Heffernan A. Clinical pharmacology: opioids. In: Macintyre PE, editor. Clinical pain management (acute pain). 2nd edition.London: Hodder & Stoughton Limited; 2008. p. 68–79.
- Duthie, D.J. and W.S. Nimmo, Adverse effects of opioid analgesic drugs. Br J Anaesth, 1987. 59(1): p. 61-77.
- Eray, O., et al., Intravenous single-dose tramadol versus meperidine for pain relief in renal colic. Eur J Anaesthesiol, 2002. 19(5): p. 368-70.
- Hazhir, S., Y.A. Badr, and J.N. Darabi, Comparison of intranasal desmopressin and intramuscular tramadol versus pethidine in patients with renal colic. Urol J, 2010. 7(3): p. 148-51.
- Latta, K.S., B. Ginsberg, and R.L. Barkin, Meperidine: a critical review. Am J Ther, 2002. 9(1): p. 53-68.
- DeLaney, M. Three Reasons Not to Prescribe Tramadol. . 2015 12/01/2019]; Available from: http://empharmd.blogspot.com/2015/05/three-reasons-not-to-prescribe-tramadol.html.
- O'Connor, A., S.A. Schug, and H. Cardwell, A comparison of the efficacy and safety of morphine and pethidine as analgesia for suspected renal colic in the emergency setting. J Accid Emerg Med, 2000. 17(4): p. 261-4.
- Jasani, N.B., R.E. O'Conner, and J.K. Bouzoukis, Comparison of hydromorphone and meperidine for ureteral colic. Acad Emerg Med, 1994. 1(6): p. 539-43.
- Mazer-Amirshahi, M., S. Motov, and L.S. Nelson, Hydromorphone use for acute pain: Misconceptions, controversies, and risks. J Opioid Manag, 2018. 14(1): p. 61-71.
- Safdar, B., et al., Intravenous morphine plus ketorolac is superior to either drug alone for treatment of acute renal colic. Ann Emerg Med, 2006. 48(2): p. 173-81, 181 e1.
- Hosseininejad, S.M., et al., Efficacy and Safety of Combination Therapy with Ketorolac and Morphine in Patient with Acute Renal Colic; A Triple-Blind Randomized Controlled Clinical Trial. Bull Emerg Trauma, 2017. 5(3): p. 165-170.
- Belkouch, A., et al., Does intranasal fentanyl provide efficient analgesia for renal colic in adults? Pan Afr Med J, 2015. 20: p. 407.
- Bektas, F., et al., Intravenous paracetamol or morphine for the treatment of renal colic: a randomized, placebo-controlled trial. Ann Emerg Med, 2009. 54(4): p. 568-74.
- Serinken, M., et al., Intravenous paracetamol versus morphine for renal colic in the emergency department: a randomised double-blind controlled trial. Emerg Med J, 2012. 29(11): p. 902-5.
- Azizkhani, R., et al., Comparing the analgesic effect of intravenous acetaminophen and morphine on patients with renal colic pain referring to the emergency department: A randomized controlled trial. J Res Med Sci, 2013. 18(9): p. 772-6.
- Masoumi, K., et al., Comparison of clinical efficacy of intravenous acetaminophen with intravenous morphine in acute renal colic: a randomized, double-blind, controlled trial. Emerg Med Int, 2014. 2014: p. 571326.
- Haddadi, S., et al., Comparing the duration of the analgesic effects of intravenous and rectal acetaminophen following tonsillectomy in children. Anesth Pain Med, 2014. 4(1): p. e13175.
- McGhie J, Serpell MG. Clinical pharmacology: local anesthetics. In: Macintyre PE, Walker SM, Rowbotham DJ, et al, editors. Clinical pain management (acute pain). 2nd edition. London: Hodder & Stoughton Limited; 2008. p. 113–29.
- Soleimanpour, H., et al., Parenteral lidocaine for treatment of intractable renal colic: a case series. J Med Case Rep, 2011. 5: p. 256.
- Motov, S., et al., Pain management of renal colic in the emergency department with intravenous lidocaine. Am J Emerg Med, 2018. 36(10): p. 1862-1864.
- Soleimanpour, H., et al., Effectiveness of intravenous lidocaine versus intravenous morphine for patients with renal colic in the emergency department. BMC Urol, 2012. 12: p. 13.
- Firouzian, A., et al., Does lidocaine as an adjuvant to morphine improve pain relief in patients presenting to the ED with acute renal colic? A double-blind, randomized controlled trial. Am J Emerg Med, 2016. 34(3): p. 443-8.
- LOJ, E.S., et al., Safety and Efficacy of Intravenous Lidocaine for Pain Management in the Emergency Department: A Systematic Review. Ann Emerg Med, 2018. 72(2): p. 135-144 e3.
- Gao M, Rejaei D, Liu H. Ketamine use in current clinical practice. Acta Pharmacol Sin. 2016;37(7):865–72.
- Kurdi, M.S., K.A. Theerth, and R.S. Deva, Ketamine: Current applications in anesthesia, pain, and critical care. Anesth Essays Res, 2014. 8(3): p. 283-90.
- Abbasi, S., et al., Can low-dose of ketamine reduce the need for morphine in renal colic? A double-blind randomized clinical trial. Am J Emerg Med, 2018. 36(3): p. 376-379.
- Hosseininejad, S.M., et al., Comparing the analgesic efficacy of morphine plus ketamine versus morphine plus placebo in patients with acute renal colic: A double-blinded randomized controlled trial. Am J Emerg Med, 2019. 37(6): p. 1118-1123.
- Farnia, M.R., et al., Comparison of intranasal ketamine versus IV morphine in reducing pain in patients with renal colic. Am J Emerg Med, 2017. 35(3): p. 434-437.
- Mozafari, J., et al., Comparing intranasal ketamine with intravenous fentanyl in reducing pain in patients with renal colic: A double-blind randomized clinical trial. Am J Emerg Med, 2019.
- Moore, C.L., et al., Imaging in Suspected Renal Colic: Systematic Review of the Literature and Multispecialty Consensus. Ann Emerg Med, 2019. 74(3): p. 391-399.
- Mefford, J.M., et al., A Comparison of Urolithiasis in the Presence and Absence of Microscopic Hematuria in the Emergency Department. West J Emerg Med, 2017. 18(4): p. 775-779.
- Coll, D.M., M.J. Varanelli, and R.C. Smith, Relationship of spontaneous passage of ureteral calculi to stone size and location as revealed by unenhanced helical CT. AJR Am J Roentgenol, 2002. 178(1): p. 101-3.
- Schoenfeld, E.M., et al., Association of Patient and Visit Characteristics With Rate and Timing of Urologic Procedures for Patients Discharged From the Emergency Department With Renal Colic. JAMA Netw Open, 2019. 2(12): p. e1916454.
- Hollingsworth, J.M., et al., Alpha blockers for treatment of ureteric stones: systematic review and meta-analysis. BMJ, 2016. 355: p. i6112.