Ch. 3 - Utilization of Emergency Services
Gregory H. Tanquary, DO, MBA; Christopher Evans, DO; Andrew Little, DO
Emergency department utilization in the United States has increased by more than 40% in the past 30 years.1 Because of a perception that emergency care is costly, the attention of government legislators, hospital administrators, insurance companies, and emergency medicine organizations has been focused on the escalating volumes. Despite concerns from regulators, patients continue to access emergency services at increasing rates for acute care needs with higher disease burden.
Emergency care and the utilization of services is changing dramatically: EDs are seeing more patients, with more complex health conditions.
Patient Demographics
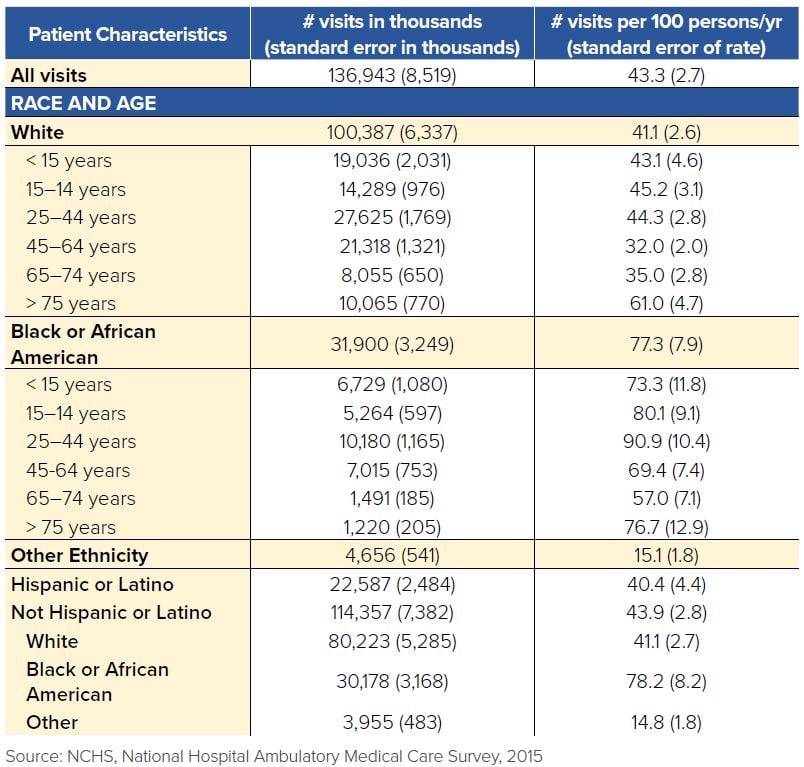
Emergency medicine spans diverse patient populations, as illustrated by the National Hospital Ambulatory Medical Care Survey (NHAMCS) in 2015.2 The highest ED users were patients from age groups 25-44 (28.6%), were female (55.4%), and were Caucasian (58.6%). Medicaid coverage was used most often (34.8%), followed by private insurance (34.3%), Medicare (17.7%), and the “other” category, which included no insurance (9.8%), patients utilizing both Medicaid/Medicare (3.6%), and worker’s compensation (0.9%).
TABLE 3.1. ED Visits by Race, Age, and Ethnicity, 20152
The relationship between ED utilization and having health insurance is complex. Two separate theories prevail. One theory is that having health insurance reduces the out-of-pocket ED costs to patients, thereby increasing ED visits. The other theory is that having health insurance encourages patients to use outpatient services, thereby decreasing ED visits. The data support both hypotheses.
In 2008 Oregon awarded Medicaid to citizens in a lottery fashion. They subsequently followed the health care utilization habits of those who acquired coverage through the lottery compared to those who did not acquire Medicaid. The results showed that obtaining Medicaid resulted in a 40% increase in ED utilization.3 A follow-up study demonstrated that these results remained consistent even 2 years later.
Conversely, a study that evaluated Kentucky’s Medicaid expansion and Arkansas’s Affordable Care Act expansion from 2013 to 2015 found opposite results. This study showed that expanding state-funded insurance programs resulted in an increased use of outpatient services by 12.1 percentage points and a decrease in ED visits by 29%.4
These conflicting results likely stem from the fact that health care benefits provided by government-funded insurance programs vary significantly from state to state with respect to deductibles, co-pays, and ED visit coverage. This makes the effects of expanding these programs exceptionally difficult to predict and apply to other states. The debate will likely remain unclear until a more homogenous system is adopted nationwide. Continued evaluation of the relationship between ED utilization and health insurance is essential as the dependence on ED services grows annually.
Increasing Utilization of EDs
Utilization of emergency department services has steadily increased over the past several years, demonstrating a growing need for the skill set emergency physicians offer. To help explain the increase in ED utilization in the U.S., the RAND Corporation performed an extensive mixed-methods study.
The analysis showed that between 2003 and 2009, direct admissions by primary care physicians (PCPs) decreased by 10%, yet the total number of hospital admissions increased.5 Delving into this discrepancy, the data showed that a 17% increase in admissions from unscheduled ED visits accounted for nearly all of the hospital admission growth.5 This pattern suggests that outpatient providers started directing their patients to EDs and relying on ED providers to determine their patients’ dispositions. The RAND Corporation interviewed PCPs, and many admitted to this phenomenon, commonly because of illness severity, patient complexity, need for after-hours care, and availability of advanced diagnostic equipment.
Walk-in patients are another common source of ED visits. The RAND study found that most individuals who presented to the ED for a non-emergent health problem did so because they perceived their illness to be life-threatening or felt they had no viable alternative.5 Many patients reported feeling they cannot contact their PCP easily. These findings suggest that efforts to reduce nonemergent ED visits should focus on timely access to PCPs, an adaptation that could reduce health care costs.
Changing Disease Severity
Our population is growing older and older. A byproduct of this is increased disease chronicity, severity, and complexity. The brunt of increased chronic disease prevalence and severity is felt on the front lines in emergency departments. It is no secret that emergency providers are expected to have
expert knowledge in a much wider range of pathology than ever before. As patients live longer with more complex health care needs, medical charting and billing must evolve as well.
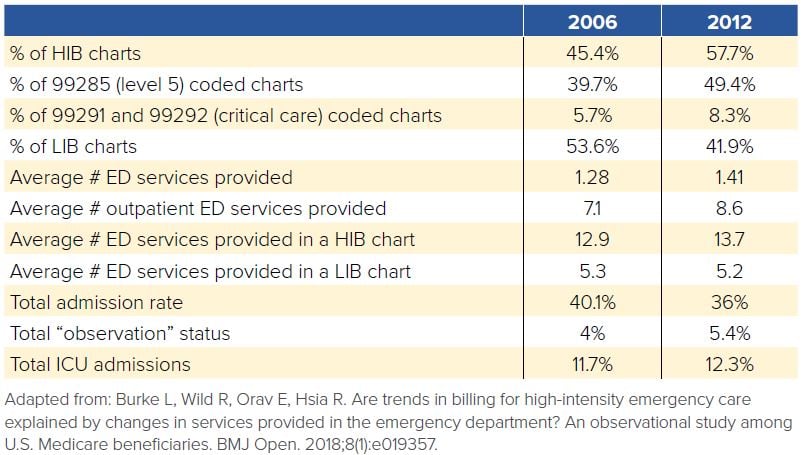
ED bills are expensive compared to a primary care visit, with patients paying a premium price for immediate care and results. While this may come at an increase cost, ED care does have the benefit of identifying life-threatening illness immediately. Unfortunately, with the steady rise in health care costs straining state and federal budgets, ED billing has received heightened scrutiny, particularly because there has been an increase in the number of high intensity billing (HIB) charts.6
HIB charts are those billed at a “level 5” or critical care level, considered to be the highest billable level of charting. Some have stipulated that the advent of the electronic health record (EHR) has facilitated this trend by making it easier for ED providers to transform a low intensity billing (LIB) chart into a HIB chart even when providing the same services. Burke et al. evaluated this contention and demonstrated that HIB charts appropriately corresponded to:6
- An increase in the number of ED services provided (laboratory tests, imaging studies, procedures)
- An increase in the number of patient comorbidities
- Higher patient complexity
- More ICU admissions
- A decrease in the number of hospital admissions
These findings suggest the ED has evolved to become a site that provides more comprehensive care to patients, thereby reducing the need for admission and justifying the increase in HIB charts.
TABLE 3.2. HIB Charts in the ED
Utilization Challenges from Hospital Closures
Unique to medicine, emergency departments are required by law to offer consultation and treatment to patients. While emergency physicians pride themselves on the credo “anybody, anytime, anywhere,” this does create a payer mix largely out of the control of EDs. Furthermore, it creates unique utilization challenges moving forward.
EDs operate under a fee-for-service model, making them lucrative businesses if their customers can pay. But EDs also operate under the Emergency Medical Treatment and Labor Act (EMTALA), meaning they must see all patients, regardless of ability to pay. EDs that serve mainly low-income and uninsured populations have therefore become financial sinkholes closing at an increasing rate, leaving the underserved communities with reduced access to emergent medical care.6-8 Since 1990 the total number of annual ED visits in the U.S. has increased by more than 40%, but the total number of EDs has decreased by 11%.7
In California, from 1990 to 2009, the total number of EDs decreased by 27%.7 Hsia et al. evaluated the characteristics of those EDs and found closures were more common if they provided services for a higher proportion of MediCal patients, served a higher proportion of black patients, and if the hospitals were for-profit.8 ED closures result in increased EMS travel times to the nearest ED, which is particularly detrimental for those who require rapid intervention, such as trauma and AMI patients.
Trauma center closures in the U.S. have mirrored ED closure trends. Between 1990 and 2005, 339 of the 1,125 trauma centers nationwide closed.9 Strikingly, only 66 closed in the decade prior.9 Hsia et al. compared transport times to the nearest trauma center in the years 2001 and 2007. They found that 24% of Americans had to travel farther to reach a trauma center in 2007 than they did in 2001; 23% of those Americans suffered an increased travel time of greater than 30 minutes.7-8 Unsurprisingly, rural districts and communities with predominantly poor, uninsured, or black populations were more at risk of nearby trauma center closure.8
Impact of ED Closures on Patient Outcomes
ED closures have become a dangerous trend, particularly because they disproportionately affect already underserved communities. This shift not only limits patient access to critical health care services, but also has the indirect effect of increasing EMS transportation times to the nearest ED.
Crandall et al. focused specifically on the effect of transport times on mortality in Chicago gunshot wound patients. They found that patients who sustained a wound greater than 5 miles from a trauma center had both increased transport times and higher mortality, but could not prove a causal relationship between those two because of uncontrollable confounding variables.9
However, Shen et al. did successfully demonstrate that relationship when they compared prehospital travel times for AMI patients in 2001 to those in 2013.7-8,10 They showed that an increased travel time to the nearest hospital by just 10 minutes correlated with a statistically significant increase in mortality at 90 days and at one year.8 Moreover, AMI patients in communities that experienced a travel time increase greater than 30 minutes had a 30% higher 90-day mortality and 21% higher one-year mortality compared to communities that experienced no increase in travel time.8 Notably, low-income populations were 9.5 times more likely to have travel time increases greater than 30 minutes.
These studies share a common theme: The majority of patients suffering from ED and trauma center closures resulting in increased transport times are disproportionately poor, black, and uninsured. Reducing access to emergency services can have detrimental effects on patient outcomes, yet it is becoming increasingly prevalent.
WHAT’S THE ASK?
Emergency care and the utilization of services is changing dramatically. To be an
effective advocate it is important to understand:
- Annual ED visits are increasing while total number of ED and trauma centers are decreasing resulting in worse patient outcomes.
- Because many patients who seek ED care for non-emergent complaints do so as a result of limited access to their PCPs, efforts should be made to increase access to PCPs.
- EDs are caring for more complex patients and delivering and billing for a higher level of care.




