Ch. 29 - Women's Health
Rosalia Holzman, MD; Casey L. Lawson, MD; Kathleen Cowling, DO, MS, MBA, FACEP
Policy and social constraints have heavily influenced both reproductive health care and women’s health care in general. Researchers are increasingly investigating gender and sex-based disparities in disease diagnosis, treatment options, and outcomes across all areas of
care, including emergency medicine. Women’s health encompasses the science needed to provide appropriate medical and reproductive care that also addresses women’s relationships, home, and work lives. The reach of women’s health goes beyond research and reproductive health topics to the very core of social biases regarding women.
Research is demonstrating significant sexbased physiologic differences in acute presentations of emergent conditions that had previously been unrecognized.
Gender-Specific Emergency Medicine
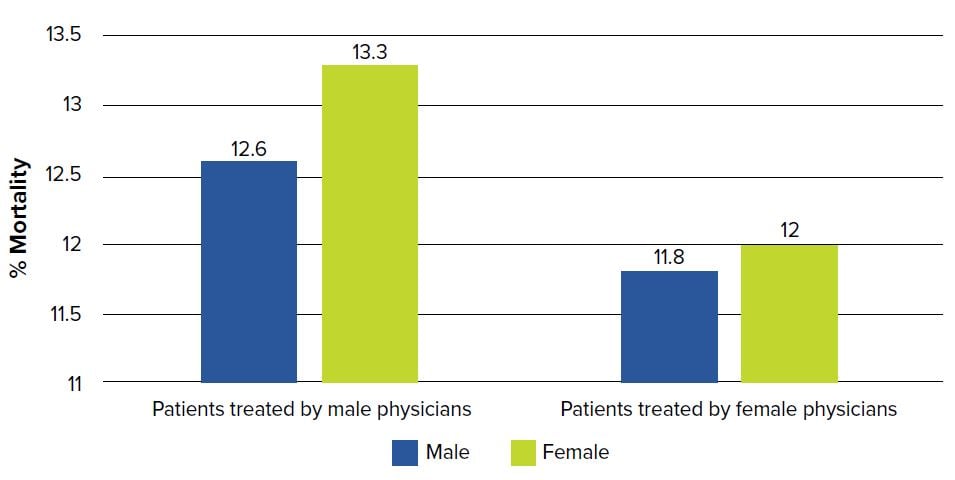
Cardiovascular disease is the No. 1 cause of death in the United States for men and women. Advances in prevention, diagnosis, and treatment have led to a decline in mortality; however, this benefit has more impact in the male population. In fact, over the past 3 decades, for women under age 55 there has been an increase in mortality from heart disease.1,2 Studies show higher mortality after a myocardial infarction (MI) in younger women compared to their male counterparts, even after accounting for differences in medical history, the severity of the infarct, and early management.3 Interestingly, recent data also demonstrates a sex-based difference in mortality based on the gender of the treating physician.4 Overall, there was improved mortality in patients suffering from an MI who were treated by female physicians. In one study, male patients treated by a male physician had a 12.6% mortality rate and female patients treated by a male physician had a 13.3% mortality rate.4 However, if the patients were treated by a female physician, they had an 11.8% and a 12% mortality rate, respectively.4 This data shows how outcomes can vary significantly by sex, and also shows that the gender of the treating physician can have an impact. This may demonstrate an unconscious gender bias toward female patients that female physicians are more frequently able to avoid.
FIGURE 29.1. Patient-Physician Gender and Mortality After Myocardial Infarction3
There is growing evidence of significant sex-based differences in the pathophysiology behind common, acute, and emergent conditions.5 This leads to variation in the time to diagnosis and mortality of various illnesses diagnosed and treated in the ED, including cardiovascular disease, COPD, and neurologic emergencies.
Emerging studies are finding variability in the risk different factors confer. Little is understood about sex-based variances in risk scores we use for acute coronary syndrome.5 Estrogen has been understood to have cardiovascular protective benefits, decreasing pre-menopausal women’s overall risk for cardiovascular disease. It is generally understood tobacco use increases risk for cardiovascular disease, but as nicotine down-regulates estrogen, it comparatively increases a woman’s risk more than a man’s.5 Women with migraines or on oral contraceptives have an increased risk for ischemic stroke and should make providers cautious with the use of vasoactive agents such as triptans.5
Women sometimes experience a delay in the diagnosis of disease due to their gender. As the number of female smokers increased, there was a subsequent increase in the incidence of COPD, which had historically been a more common diagnosis among men.5 Without recognizing this change, some women experienced a delay in their diagnosis of COPD as they were referred by physicians for testing less frequently than men.6 This lack of testing could result in misdiagnosis or delay of appropriate care for the affected women when they present to the ED with undifferentiated respiratory distress. Women are also referred less often for cardiac testing such as stress tests and cardiac catheterizations when they present with potential symptoms of ACS.5 In addition, women in atrial fibrillation are less frequently started on anticoagulation, likely conferring an increased risk of future ischemic stroke. Women with ischemic stroke experience longer door-to-treatment times and are treated less frequently with tissue plasminogen activator.5 Research continues to demonstrate significant sex- and gender-based differences in many other areas, and it is important to remain informed of these distinctions to provide better care and improve patient outcomes.
Historical Barriers to the Inclusion of Females in Research
Historically, research studies have been focused on men. An FDA guideline in 1977 urged the exclusion of women of “child-bearing potential” from clinical trials except in life-threatening conditions.7 Caucasian males were the “norm” study population, and women were assumed to be an expensive test group, in part due to fluctuating hormone levels.7,8 This hindered physicians’ ability to properly diagnose, educate, and treat women. It wasn’t until the 1980s that the medical community realized its quality and quantity of knowledge about women’s health was lacking.
The FDA released a guidance statement in 1993 encouraging gender inclusion in early clinical trials.9 It was intended to be used as a drug development industry guidance standard. This new guideline came about because of concerns from the scientific community (including physicians, researchers, pharmacists, and drug manufacturers) that the effects of drugs on female physiology were not understood due to a paucity of information. Even many years after this ban was lifted, in 2001, a review of clinical trials found that almost 90% of researchers did not conduct gender-specific analysis.10 For example, heart disease is the leading cause of death for women in the United States, but only about 20% of enrolled patients in CVD research studies are women.11,12
Women’s exclusion from clinical trials and their grouping along with men during data analysis affects the way that we practice medicine today. Emergency physicians can change this and be the springboard for pointing out sex and gender differences across many areas of medicine. Many of the diseases seen in the ED every day have subtle differences based on gender. Gender-specific medicine is about improving care for men and women, boys and girls, using knowledge of different risk factors and medication responses.
Sex and gender disparities exist in the participation of female patients in research, and also in the numbers of female researchers. Across the globe, as of June 2018, headcounts of persons employed in research and development show that less than 30% of researchers are women.13 Women who conduct research are paid less, publish less, and largely do not progress forward with their careers to the same extent that men do, which may be in part due to bias regarding publication in journals with high impact factors.14,15 It is critical that more women are recruited into medicine and science, and that subtle biases and prejudices are avoided to ensure that men and women receive the same opportunities, teaching, and mentorship.
Access to Reproductive Health Care
The ACA aimed to improve access to health care for all Americans, both men and women. It addressed issues such as pre-existing conditions, along with women’s health — including access to preventive health care. All health care plans are required to cover specific essential health benefits including pregnancy, maternity, and newborn care, along with preventive services16 like health screenings (such as lab tests for sexually transmitted infections and anemia), contraception, and well-women visits. Under the ACA, the number of
insured women of reproductive age increased.17 Improved access to insurance and preventive services led to improved public health, including a reduction in unintended pregnancies.18,19
An important indicator of national health is infant mortality. The United States’ infant mortality rate remains higher than most other developed countries20 and the most common causes of infant mortality include preterm birth, low birth weight, and birth defects.21 Many of these outcomes can be prevented or managed early when expectant mothers have access to proper prenatal care. Between 2010 and 2016, improved rates in infant mortality were noted in states that accepted Medicaid expansion under the ACA, further demonstrating the importance of access to prenatal care to reduce infant mortality.22
Many uninsured women (especially those who are young or low-income) rely on publicly funded or nonprofit services (such as those associated with Planned Parenthood) for family planning. State policy changes in Texas decreased funding for these family planning services. This change created the opportunity to analyze the effect of these services on women’s health. In the 4 years after financial cuts to the federally-funded family planning clinics in specific Texas counties, there was a 3.4% increase in teen birth rates.23 Texas also passed a law placing restrictions on abortion centers, requiring physicians providing abortions to have admitting privileges at hospitals, and requiring facilities providing abortions to meet the standards of ambulatory surgical centers; the same law restricted medical abortions and banned abortions after 20 weeks.24 These changes led to closure of 31 out of 41 abortion-providing facilities in the state, thus reducing the geographic distribution of these facilities and more than quadrupling the wait times women experienced, from 5 days to 21 days or longer.24 The repercussions were many, including an increase in the number of abortions performed after 12 weeks’ gestation, leading to higher risk of complications.25 Emergency providers directly see effects of these barriers when caring for women who may not have had adequate health screenings, proper access to prenatal care, or who are dealing with unintended pregnancies.
Intimate Partner Violence
Intimate partner violence (IPV) is a serious public health issue that profoundly impacts the lives of patients in the ED. More than 1 in 3 women in the United States will experience IPV in their lifetime.26 IPV includes physical or psychosocial abuse, stalking, threats of harm and intimidation, and rape. By contrast, the number of women who will experience invasive breast cancer is 1 in 8.27 The social and economic costs of IPV are enormous. Emergency physicians must advocate for both men and women who suffer from IPV.
It is not enough to ask patients if they are safe at home only after identifying trauma, bruising, or other marks that are suspicious. Screening protocols are vital in identifying victims of IPV. Identification of victims of IPV by physicians is low, even though most women state they would be comfortable telling a physician about their experience with IPV.24 Further, screeners, whether they are triage nurses or physicians, must be educated on appropriate ways to respond. Many modern EDs are crowded with boarding patients and hallway beds, making screening even more challenging, as it should be done in a private place without any visitors.25
Once a patient has divulged s/he is experiencing IPV, a few critical actions are necessary. It is imperative to ask if the patient feels safe to return home and if there are any children in the home who may be at risk or also experiencing abuse. Emergency physicians should provide resources for these patients, such as information about domestic violence shelters in the area that can provide alternate housing; social workers can be an invaluable resource in providing these materials. In addition, emergency physicians should ask if the patient would like to report the abuse to law enforcement. While elder and child abuse must be reported in all 50 states, the same is not true for IPV. Future policy and advocacy efforts could focus both on optimizing screening for IPV and improving the ease of reporting without putting the women at greater risk.
Sexual Assault Nurse Examiners (SANE) play a critical role in IPV treatment and forensic evidence collection. After a victim of rape or sexual abuse has reported abuse, it is incredibly important that, as emergency physicians, we provide them with the support and care they need and deserve without re-victimizing them. SANE nurses play a crucial role because they are well trained to perform evidence collection, as well as provide support, care coordination and follow up. In addition, SANE evidence is the strongest evidence for victims in the courtroom.26,27 However, some facilities do not offer access to SANE nurses for their emergency physicians, possibly because of cost (especially for facilities that do not have large volumes of patients). In this instance, it is important to seek the policy and practice information needed to treat and care for victims of IPV. The paper titled “Managing Intimate Partner Violence in the Emergency Room” by Dr. Esther Choo and Dr. Debra Houry25 is a suggested resource.
Summary
Research is demonstrating significant sex-based physiologic differences in acute presentations of emergent conditions that had previously been unrecognized, affecting women’s access to necessary testing and treatment. Emergency physicians can make a significant difference in this arena by conducting research that involves women and analyzing this data separately to improve clinical outcomes across a wide array of potentially life-threatening conditions. Federal and state policies also impact women’s health in both access to reproductive health services and appropriate care for patients experiencing intimate partner violence. Emergency physicians can play an important role in advocating for improved screening, resources, and awareness of intimate partner violence and learn about available resources in the geographical areas where they practice.
WHAT’S THE ASK?
- Advocate for mentorship for women in your practice and equitable evaluation practices for all members of your team, regardless of gender.
- Conduct and advocate for research that analyzes gender and sex differences.
- On a state and federal level, advocate for access to women’s health services and improved screening and resources for patients facing IPV.




